UDK: 616.24-085.816.2:616.12-073.432.19
Naumovski F.1; Shosholcheva M.2; Cholanchevski R.3; Andonovska B.1; Trajkovska Dz.V.1; Jovanovski Srceva M.1
1University Clinic for Traumatology, Orthopedics, Anesthesiology, Reanimation, Intensive Care and Emergency Department – Skopje, Department of Anesthesiology, Reanimation and Intensive Care, “Ss Cyril and Methodius” University – Skopje
2University Clinic of Surgical Diseases “St. Naum Ohridski” – Skopje, Department of Anesthesia and Intensive Care – Skopje, “Ss Cyril and Methodius” University – Skopje
3University Clinic for Thoracic and Vascular Surgery – Skopje, Department for Thoracic Surgery, “Ss Cyril and Methodius” University – Skopje
Abstract
Pulmonary contusions mediated immunological lung injury characterized with interstitial involvement, as well as therapeutically applied positive pressures over the already damaged alveoli could lead to elevation of the pressures inside pulmonary circulation. Fifty patients were included in the study and divided into two groups, whereby 26 were mechanically ventilated while 24 were spontaneously breathing patients. In all patients Pulmonary Capillary Wedge Pressure (PCWP) was measured non-invasively using echocardiography. Measurements of Left Atrial Pressure (LAP) were made 24 hours after admission, on the 7th and 14th day of admission in the ICU. PCWP was calculated using the LAP values and the Nagueh formula (LAPx1.24+1.98). Lung ultrasound was used for the measurement of severity of the lung injury according to the BLUE Protocol. Mean values for PCWP were calculated in both groups and the difference was examined using the Student T Test. It was found that the values for PCWP did not differ significantly between the groups when measured 24 hours and 7 days after admission and mechanical ventilation initiation (t = -0.11 and 1.13 for value for p 0.45 and 0.13),but were significantly higher in mechanically ventilated patients after 14 days of mechanical ventilation commencement (mean 10.52 vs. 7.88, t=1.89 for p of 0.03). Lung injury in patients with pulmonary contusions, as well as inflammation during the process of damage and repair, involves interstitial changes which can lead to affection of small pulmonary vessels as well. Therapeutically applied positive pressure ventilation and alveolar distension could impair blood flow through small pulmonary capillaries and vessels. When both combined, they can lead to elevation of small circulation pressures. Mechanical ventilation in patients with pulmonary contusions is associated with higher PCWP after 14 days of positive pressure ventilation in comparison to spontaneously breathing patients. Duration of mechanical ventilation is associated with higher levels of PCWP.
Key Words: Mechanical ventilation; PCWP; Pulmonary contusions.
Introduction
Pulmonary contusions are frequently met in polytraumatized patients demanding admission in the Intensive Care Unit. Approximately 25-80% of patients with chest trauma develop pulmonary contusion which is considered as a serious morbidity and mortality predictor (1). After trauma occurrence which implies kinetic energy transfer over the lung, according to Kurt A. et al., the second attack of the lung is mediated by the exaggerated immunologic response involving cytokines and proinflammatory mediators release leading to generalized lung injury (2). Therefore, inflammation mediated capillary leak leads to higher vascular permeability and leucocyte migration outside the pulmonary vasculature into interstitial space and into alveoli impairing gas exchange. Impaired gas exchange by itself leads to elevation of pulmonary vascular resistance, and in some cases, it demands mechanical ventilation with positive pressure which additionally can have negative impact over pulmonary circulation. According to abovementioned facts we assume that mechanical ventilation in patients with pulmonary contusions can have deleterious effects over the heart and systemic hemodynamics. Therefore, left atrial pressure (LAP) was assessed using echocardiography in both mechanically ventilated and spontaneously breathing patients in order to calculate Pulmonary Capillary Wedge Pressure (PCWP) since LAP can be measured using echocardiography and PCWP can be calculated using equitation of Nagueh with high accuracy (3,4).
Aim of the Study
The aim of this study is to reveal does PCWP in patients with pulmonary contusions differ significantly in between mechanically ventilated versus spontaneously breathing patients. It is expected that the results of this study will help in understanding does mechanical ventilation when applied possesses additional negative effect over the already injured lungs. Since lung injury by itself could be related to changes in PCWP, we have measured Lung Ultrasound Severity Score (LUSS) in order to quantify the severity of lung contusion and to examine the possible relationship between LUSS and PCWP.
Material and Methods
In total, 50 polytraumatized patients with pulmonary contusions were included in this study. All patients that were included in the study had signed informed consent by a family member since some of them were sedated and unconscious. All patients that we had a signed informed consent for and were older than 18 years of age fulfilling the inclusion criteria were included in the study. Pulmonary contusions without pneumothorax were detected with computed tomography which has been evaluated by a radiologist prior to patient’s admission in the ICU. Patients who were previously resuscitated, with already known pulmonary hypertension or heart pathology, with pneumothorax or pregnant women were excluded from the study. The study was conducted at the Clinical Campus “Mother Theresa” in Skopje at the University Clinic for Traumatology, Orthopedics, Anesthesia, Reanimation, Intensive Care and Emergency department – Skopje at the Department of Anesthesiology, Reanimation and Intensive Care. Conduction of this study was approved by the Ethical Committee for Human Research of Medical Faculty – Skopje at “Ss Cyril and Methodius” University – Skopje on 1st of February 2023 with number of approval 03-300/3. All patients were divided regarding the need for mechanical ventilation into two groups, a mechanically ventilated and spontaneously breathing group. Echocardiographic examination was performed in all participants 24 hours after admission, 7 days after admission and 14 days after admission. In order to calculate Pulmonary Capillary Wedge Pressure (PCWP), it was examined the left ventricle according to the Recommendations for Cardiac Chamber Quantification by Echocardiography in Adults published by the American Society of Echocardiography and the European Association of Cardiovascular Imaging (5). Firstly, transmitral pulse wave doppler has been used in order to detect transmitral E/A (Figure 1A). Afterwards, with usage of Tissue Doppler, e’ was detected and measured using Pulse Wave Doppler (Figure 1B). Measured values for E and e’ when divided as in the equitation E/e’, gave us the value for LAP. Consequently, LAP was used for calculation of PCWP according to the Nagueh equitation (3,4). PCWP is equal to LAPx1.24+1.98 and it has been already proven that can be substitute of invasively measured PCWP without significant difference and with satisfying accuracy (3,4). From the measured values, mean PCWP was calculated in both mechanically ventilated versus spontaneously breathing patients, while the difference between them was examined using the Student T Test.
A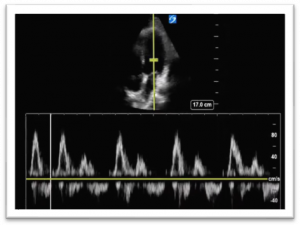 |
B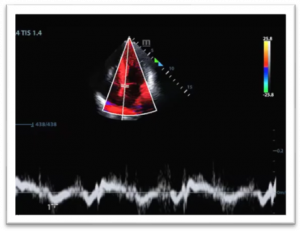 |
Figure 1. Transmitral Pulse Wave Doppler whit tracing of E and A waves (1A) and measurement of Septal e’ with tissue doppler and Pulse wave Doppler (1B).
At the same examining points when LAP and PCWP were measured, LUS Score was measured, as well. LUS Score was measured by performing an ultrasonographic examination of both lungs divided in total 12 segments or 6 of them in each lung according to Lichtenstein’s Protocol (6). Upper anterior, lateral and posterior and lower anterior, lateral and posterior segment in each lung were scanned with curvilinear probe in order to assess the severity of lung contusion. Normal aeration was seen as the presence of A-lines which are parallel to the pleural line and were scored with 0 points (Figure 2A). The existence of interstitial syndrome because of capillary leak was recognized when 3-5 B-lines were seen at any part of the lung scoring them as 1 point (Figure 2B). When more than 5 B-lines were detected or multiple B-lines were present, the existence of alveolo-interstitial syndrome was established and scored with 2 points (Figure 2C). The presence of dense consolidations with a hepatic or tissue-like structure were scored with 3 points (Figure 2D). All scanned segments in total were referred to as Lung Ultrasound Severity Score (LUSS) which could vary from 0-36 depending on the injury heaviness. Mean LUS Scores have been calculated for all examining points, and we compared them in between mechanically ventilated versus spontaneously breathing patients. In order to understand does the severity of lung injury exemplified by LUSS could have an impact over the PCWP correlation between those two variables 24 hours after admission, 7 days and 14 days after admission, it was assessed with Pearson’s Correlation Test.
A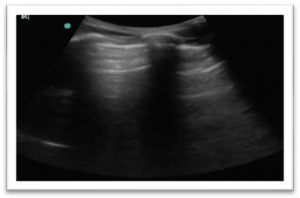 |
B |
C |
D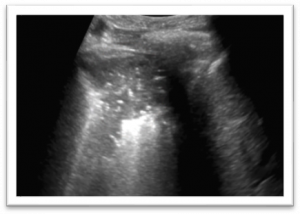 |
Figure 2. Ultrasonographic findings of pulmonary ultrasound: Figure 2A. Presence of A-lines showing good aeration of the lung scored with 0 points; Figure 2B. Presence of B-lines scored with 1 point; Figure 2C. Presence of multiple B-lines with their confluence scored with 2 points and Figure 2D. Pulmonary consolidation scored with 3 points according to LUSS.
Results
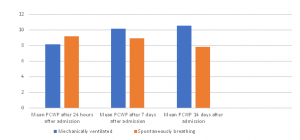
Among the 50 polytraumatized patients that were included in the study, 26 of them (52%) were mechanically ventilated, versus 24 (48%) who were in the spontaneously breathing group not needing mechanical ventilation. According to the values for measured LAP and calculated PCWP, we did not find statistically significant difference between groups 24 hours after admission (Mean PCWP: 8.09 versus 9.12; Student T-test: t=-1.2 and p 0.11). Nevertheless, of not existing significant difference 7 days after admission, we found that mean values for PCWP were higher in mechanically ventilated patients (mean PCWP: 10.15 versus 8.91; Student T-test: t=1.14 and p 0.12). Fourteen days after admission we have measured significantly higher values for PCWP in mechanically ventilated patients when compared to spontaneously breathing patients (mean PCWP: 10.52 versus 7.8; Student T-test: t=1.89 and p 0.032) (Table 1 and Figure 1).
Table 1. Mean values for PCWP measured in mechanically ventilated versus spontaneously breathing patients.
| Mechanically ventilated | Spontaneously breathing | |
| Mean PCWP after 24 hours of admission | 8.09 | 9.12 |
| Mean PCWP after 7 days of admission | 10.15 | 8.91 |
| Mean PCWP after 14 days of admission | 10.52 | 7.8 |
Figure 1. Mean values for PCWP measured in
mechanically ventilated versus spontaneously breathing patients
Mean LUS Score after 24 hours of admission was 9.19 in mechanically ventilated patients versus 7.96 in spontaneously breathing patients without significant difference between both groups (Student T test: t=0.85 and p 0.198). Seven days after admission mean LUSS was 14.41 in mechanically ventilated patients versus 9.78 in spontaneously breathing patients. After 14 days of admission, we have found mean LUS of 13.26 in mechanically ventilated patients versus 5.72 in spontaneously breathing patients. According to above-elaborated results we have found significantly higher values of LUSS in mechanically ventilated patients 7 and 14 days after admission when compared to spontaneously breathing patients (Student T test: t=2.56 and p 0.0069 for measurements done after 7 days of admission; t=3.77 and p 0.00029 for measurements taken 14 days after admission) (Table 2).
Table 2. Mean values of LUSS in mechanically ventilated and spontaneously breathing patients and their comparison with Student T Test values.
| Mechanically ventilated | Spontaneously breathing | Student T Test: T value | Student T Test: p values | |
| LUSS 24 hours after admission | 9.19 | 7.96 | 0.85 | 0.198 |
| LUSS 7 days after admission | 14.41 | 9.78 | 2.56 | 0.0069 |
| LUSS 14 days after admission | 13.26 | 5.72 | 3.77 | 0.00029 |
The correlation between LUSS and measured PCWP in both groups 24 hours after examination, 7 and 14 days after admission was examined using Pearson Correlation Coefficient. The existence of positive correlation between measured LUSS and PCWP at every examination point in both groups was found. Values for correlation coefficient R in mechanically ventilated patients were 0.4; 0.17 and 0.46 for measurements made 24 hours after admission, 7 and 14 days after admission respectively. In spontaneously breathing patients values for R were 0.46; 0.373 and 0.269 respectively.
A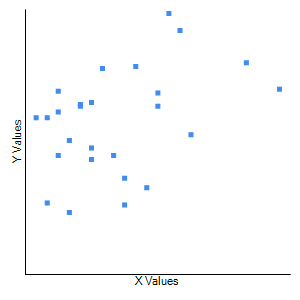 |
B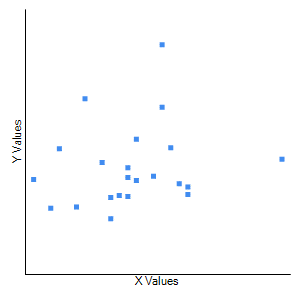 |
C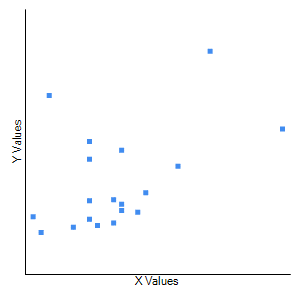 |
F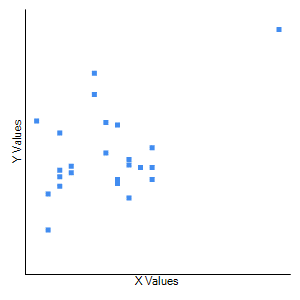 |
E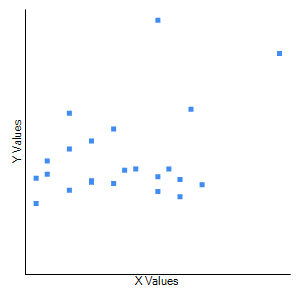 |
D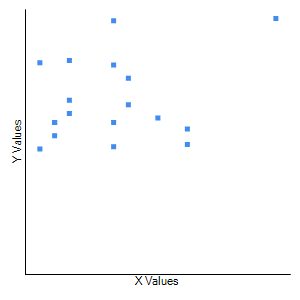 |
Figure 2. Correlation between LUSS and PCWP in mechanically ventilated patients 24 hours after admission (2A), 7 days after admission (2B) and 14 days after admission (2C) and in spontaneously breathing patients 24 hours after admission (2D), 7 days after admission (2E) and 14 days after admission (2F) (X values stand for LUSS; Y values stand for PCWP).
Discussion
Pulmonary Capillary Wedge Pressure (PCWP) has been recognized as a key factor in diseases that involve both heart and lungs. Since positive pressure ventilation adds pressure over the alveolar capillaries, it is expected to influence pulmonary circulation by exhibiting changes in pulmonary pressures including PCWP. Therefore, Souza R. et al. have examined the level of PCWP in patients with idiopathic pulmonary hypertension and compared it to patients experiencing ARDS concluding that ARDS has been associated with mild pulmonary hypertension (7). These findings justify the examination of PCWP in patients with pulmonary contusions, since most of them experience some sort of acute lung injury. Since elevated levels of PCWP were recognized in mechanically ventilated patients with respiratory insufficiency and had been clearly stated back in 1977 (8), we believe that mechanical ventilation could be another source of pulmonary injury despite the primary pulmonary damage made by the kinetic energy leading to a higher level of PCWP in mechanically ventilated patients. According to our results it was found that levels of PCWP were higher in mechanically ventilated patients after 7 days of mechanical ventilation but were significantly higher in mechanically ventilated patients after 14 days of mechanical ventilation, initiation which implies that longer lasting positive pressure ventilation is related to higher values of PCWP. In one randomized controlled trial where systolic, diastolic pulmonary artery pressure and PCWP were examined in patients with ARDS induced by pulmonary contusions versus ARDS from other origin, it was found that the patients experiencing ARDS caused by pulmonary contusions had significantly higher values for systolic and diastolic pulmonary artery pressure as well as PCWP (9). They found that PCWP is higher 72 hours after pulmonary contusion occurrence when compared to measurements at 0 and 48 hours after admission, which is in concordance with our findings that PCWP becomes higher as time passes after mechanical ventilation has been initiated. When compared to our study, the study of Yang W. et al. had examined the patients using Swan Ganz catheter and pulse index continuous cardiac output (PiCCO) monitoring while we were using non-invasive echocardiographic monitoring. Their study has provided results in timeframe of 0 to 72 hours, while ours have examined PCWP in an extended period of time up to 14 days of ICU admission. Compared to our study they have not specified if the patients were mechanically ventilated or not, but have confirmed that pulmonary contusions are associated with higher values for pulmonary circulation pressures (8). Moreover, they have found that higher values for PCWP were associated with elevated values of extravascular lung water (9) which could also be estimated when using LUS Lichtenstein’s BLUE Protocol as it was used in our study. Elevation of the amount of extravascular lung water has been related to increased microvascular permeability and due to high hydrostatic pressures (10). Regarding the relationship of the values for PCWP and the LUSS which are showing the severity of lung damage, we have found positive correlation of the measured PCWP with LUSS at 24 hours, 7 days and 14 days after admission in the ICU, which once again confirms the above-stated findings of Yang W. et al. Increased pulmonary capillary wedge pressure was met in the study of Hakim TS. et al. as well, where increasement of PEEP above 5 was associated with significant increase of PCWP elevation which confirms that positive pressure mechanical ventilation is associated with higher values for PCWP which was observed in our study when comparing to spontaneously breathing patients (11). Another study published by Slim AM and coworkers have found strong association of increased levels of PCWP in mechanically ventilated patients with positive pressure ventilation which is believed to happen not because of change in volume but rather because of elevation of intrapulmonary pressures (12). Application of continuous positive pressure ventilation in the form of nasal CPAP in patients with obstructive sleep apnea was proven to be followed by significant elevations of pulmonary pressures including PCWP which was correlated with the amount of cm of H20 of CPAP applied over the lung (13). Positive pressure ventilation in contrast to spontaneous breathing implies application of PEEP which has been already verified to be associated with higher levels of PCWP (14) which explains our results of detecting higher levels of PCWP in those patients who were mechanically ventilated. Since the mean value for LUSS in both groups 24 hours after admission did not differ significantly, we believe that the severity of pulmonary contusions was similar in both examined groups. This statement implies that the severity of the initial trauma could not be the reason why mechanically ventilated patients exhibit higher PCWP values, but rather mechanical ventilation by itself leads to elevation in PCWP in patients exposed to positive pressure ventilation. The absence of invasive measurement of PCWP could be considered as a limitation in this study since that way more precise measurements could be provided and compared to noninvasively derived measurements provided by echocardiography. Invasive monitoring of PCWP is a gold standard in complex cases, but it has been related to complications with measurement, therefore a noninvasive way of monitoring pulmonary pressures using echocardiography could be a safer source of valuable data on a daily basis in critically ill patients. Further examination of pulmonary pressures on a bigger cohort of patients may be needed in order to provide deeper information about the heart lung interactions in polytraumatized patients with pulmonary contusions.
Conclusions
Using noninvasive echocardiography derived measurements, we have found higher values for PCWP in mechanically ventilated patients with pulmonary contusions when compared to spontaneously breathing patients. According to our findings, the duration of mechanical ventilation has been associated to significantly higher PCWP values. Since we did not find any significant difference in the severity of the initial injury, we believe that initial lung injury is not related to difference in PCWP that we have found between the groups. PCWP has correlated with severity of lung injury and the amount of extravascular lung water both represented by LUSS.
References
- Hosseini M, Ghelichkhani P, Baikpour M, et al. Diagnostic accuracy of ultrasonography and radiography in detection of pulmonary contusion; A systematic review and meta-analysis. Emerg (Tehran) 2015;3:127–36.
- Kurt A, Turut H, Acipayam A, Kirbas A, Yuce S, Cumhur Cure M, Cure E. Investigation of surfactant protein-D and interleukin-6 levels in patients with blunt chest trauma with multiple rib fractures and pulmonary contusions: a cross-sectional study in Black Sea Region of Turkey. BMJ Open. 2016 Oct 12;6(10):e011797. doi: 10.1136/bmjopen-2016-011797. PMID: 27733410; PMCID: PMC5073616.
- Nagueh SF, Middleton KJ, Kopelen HA, Zoghbi WA, Quiñones MA. Doppler tissue imaging: a noninvasive technique for evaluation of left ventricular relaxation and estimation of filling pressures. J Am Coll Cardiol. 1997 Nov 15;30(6):1527-33. doi: 10.1016/s0735-1097(97)00344-6. PMID: 9362412.
- Bouhemad B, Nicolas-Robin A, Benois A, Lemaire S, Goarin JP, Rouby JJ. Echocardiographic Doppler assessment of pulmonary capillary wedge pressure in surgical patients with postoperative circulatory shock and acute lung injury. Anesthesiology. 2003 May;98(5):1091-100. doi: 10.1097/00000542-200305000-00011. PMID: 12717130.
- Roberto M. Lang, MD, FASE, FESC, Luigi P. Badano, MD, PhD, FESC, Victor Mor-Avi, PhD, FASE, Jonathan Afilalo, MD, MSc, Anderson Armstrong, MD, MSc, Laura Ernande, MD, PhD, Frank A. Flachskampf, MD, FESC, Elyse Foster, MD, FASE, Steven A. Goldstein, MD, Tatiana Kuznetsova, MD, PhD, Patrizio Lancellotti, MD, PhD, FESC, Denisa Muraru, MD, PhD, Michael H. Picard, MD, FASE, Ernst R. Rietzschel, MD, PhD, Lawrence Rudski, MD, FASE, Kirk T. Spencer, MD, FASE, Wendy Tsang, MD, Jens-Uwe Voigt, MD, PhD, FESC, Recommendations for Cardiac Chamber Quantification by Echocardiography in Adults: An Update from the American Society of Echocardiography and the European Association of Cardiovascular Imaging, European Heart Journal – Cardiovascular Imaging, Volume 16, Issue 3, March 2015, Pages 233–271, https://doi.org/10.1093/ehjci/jev014.
- Mojoli F, Bouhemad B, Mongodi S, Lichtenstein D. Lung ultrasound for critically ill patients. Am J Respir Crit Care Med.2019;199(6):701–714. doi: 10.1164/rccm.201802-0236CI.
- Souza R, Amato MB, Demarzo SE, Deheinzelin D, Barbas CS, Schettino GP, Carvalho CR. Pulmonary capillary pressure in pulmonary hypertension. Crit Care. 2005 Apr;9(2):R132-8. doi: 10.1186/cc3038. Epub 2005 Feb 11. PMID: 15774045; PMCID: PMC1175923.
- Labrousse J, Tenaillon A, Massabie P, Simonneau G, Lissac J. Influence de la ventilation artificielle sur la pression capillaire pulmonaire dans les insuffisances respiratoires aiguës (Effect of artificial ventilation on pulmonary capillary pressure in acute respiratory insufficiency). Nouv Presse Med. 1977 May 7;6(19):1639-42. French. PMID: 866151.
- Yang WJ, Zhao XF, Wei K, Feng QG, Wang W, Liu XZ. (Clinical study on pulmonary circulation changes in patients with acute respiratory distress syndrome induced by lung contusion). Zhongguo Wei Zhong Bing Ji Jiu Yi Xue. 2012 Jul;24(7):407-11. Chinese. PMID: 22748456.
- Benzing A, Geiger K. Inhaled nitric oxide lowers pulmonary capillary pressure and changes longitudinal distribution of pulmonary vascular resistance in patients with acute lung injury. Acta Anaesthesiol Scand. 1994 Oct;38(7):640-5. doi: 10.1111/j.1399-6576.1994.tb03970.x. PMID: 7839770.
- Hakim TS, Gilbert E, Camporesi E. Positive end-expiratory pressure increases capillary pressure relative to wedge pressure in the closed and open chest. J Crit Care. 1993 Jun;8(2):80-6. doi: 10.1016/0883-9441(93)90011-9. PMID: 8343866.
- Slim AM, Martinho S, Slim J, Davenport E, Castillo-Rojas LM, Shry EA. The effect of airway pressure release ventilation on pulmonary catheter readings: specifically pulmonary capillary wedge pressure in a Swine model. Anesthesiol Res Pract. 2011;2011:371594. doi: 10.1155/2011/371594. Epub 2011 Feb 24. PMID: 21403912; PMCID: PMC3049321.
- Akashiba T, Minemura H, Yamamoto H, Itoh D, Kosaka N, Saitoh O, Horie T. Effects of nasal continuous positive airway pressure on pulmonary haemodynamics and tissue oxygenation in patients with obstructive sleep apnoea. Respirology. 1999 Mar;4(1):83-7. doi: 10.1046/j.1440-1843.1999.00159.x. PMID: 10339735.
- Smiseth OA, Thompson CR, Ling H, Robinson M, Miyagishima RT. A potential clinical method for calculating transmural left ventricular filling pressure during positive end-expiratory pressure ventilation: an intraoperative study in humans. J Am Coll Cardiol. 1996 Jan;27(1):155-60. doi: 10.1016/0735-1097(95)00420-3. PMID: 8522690.