UDK: 616.13/.14-002-073.756.8:004
Andonov G.1,2, Nikolova S.1,2
1Institute of Radiology, Skopje, Republic of North Macedonia
2 Faculty of Medicine, “Ss Cyril and Methodius” University, Skopje, Republic of North Macedonia
Abstract
Behçet’s disease (BD), also called Behçet’s syndrome, is a rare multisystemic vasculitis that causes blood vessel inflammation throughout the body. It may affect multiple organs and less frequently involves the central nervous system, potentially resulting in thrombotic events and aneurysm formation, the most notably pulmonary artery aneurysms (PAA).
We present a case of a 44-years-old female who sought medical attention due to prolonged hemoptysis combined with chest pain.
Ascribed to these symptoms, initial computer tomography (CT) (native and arterial phases) revealed an oval mass in the left hilum. Subsequent CT angiography demonstrated an aneurysm of the left interlobar artery compressing the segmental bronchus with associated thrombus formation. The patient refused surgical intervention. One year later, a follow-up CT angiography showed the resolution of the initial aneurysm but revealed a new aneurysm in the right main pulmonary artery.
This case highlights the rare migratory nature of pulmonary aneurysms in Behçet vasculitis, underscoring the need for early diagnosis, imaging follow-up and interdisciplinary management.
Key Words: Behçet Vasculitis; CT angiography; case report; vascular anomalies.
Introduction
Behçet vasculitis is a rare systemic vascular inflammatory disorder resulting in aneurysms and thrombosis (1). Pulmonary artery aneurysms are serious complications, often leading to life-threatening hemoptysis. Chronic endothelial dysfunction is central to the pathogenesis of Behçet disease (2). The prothrombotic factors and impaired fibrinolysis contribute to aneurysm development and thrombus formation. Advanced imaging, particularly contrast-enhanced computer tomography (CT) angiography, plays a pivotal role in diagnosis (3).
The clinical heterogeneity of Behçet disease mandates vigilance among clinicians and radiologists. Contrast-enhanced CT angiography with a 15-seconds delay is a key tool for precise anatomical delineation (4).
Endothelial damage triggers local thrombosis, potentially leading to aneurysm rupture or embolization. Patients with Behçet disease often exhibit hypercoagulability with elevated levels of procoagulant factors and impaired fibrinolysis. This prothrombotic environment contributes to vessel thrombosis and aneurysm formation (5).
This case report aims to contribute to the literature by detailing the clinical presentation, imaging findings and management approach of a patient with Behçet vasculitis and migrating pulmonary aneurysms.
The differential diagnosis includes Hughes-Stovin Syndrome (HSS), a rare autoimmune disorder characterized by pulmonary artery aneurysms, hemoptysis, chest pain and recurrent fever. HSS, like Behçet disease, results from vasculitis causing arterial occlusion, aneurysm formation and venous involvement. The histology of the aneurysms in both conditions can be similar (1).
By presenting a detailed analysis of a real-world case, showing that most of the such cases in the epidemiologic picture were seen in Mediterranean, East European and Asian regions, we aim to enhance awareness among healthcare professionals, fostering early recognition and facilitating timely intervention to mitigate potential complications associated with venous insufficiency.
This case report not only contributes to the expanding knowledge base of vascular anomalies but also serves as a reference for future cases of Behçet syndrome.
Case Presentation
A 44-years-old female presented with complaints of recurrent hemoptysis and persistent chest pain. She had no history of significant trauma, deep vein thrombosis, coagulopathies or other predisposing vascular conditions. Her past medical history was unremarkable, and she denied recent infections or autoimmune disorders. Initial imaging was performed with a non-contrast chest CT, and an oval-shaped mass was revealed in the left hilum, raising suspicion for a vascular anomaly. Contrast-enhanced CT angiography further delineated the lesion as an aneurysm in the left interlobar pulmonary artery, measuring several millimeters in diameter. The aneurysm was compressing the adjacent segmental bronchus and was associated with thrombus formation extending into the segmental and subsegmental bronchi supplying the left lower lung lobe. Follow-up imaging (1 year later) was done: the previously noted left interlobar artery aneurysm was no longer visualized, suggesting possible spontaneous resolution or thrombosis. However, a new aneurysm was identified in the right main pulmonary artery. This new aneurysm was associated with pulmonary micro-thrombosis, raising concerns for an underlying systemic or vascular pathology predisposing to aneurysm formation. The patient was referred to rheumatologist for laboratory evaluation and systemic therapy initiation. Due to disease progression, consultation with a vascular surgeon in Vienna, Austria was arranged. However, the patient refused surgical intervention. Long-term management includes ongoing imaging surveillance and symptomatic treatment to mitigate further complications.
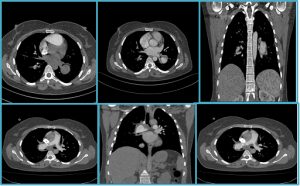
Figure 1a-c. The first three images depict aneurysm in the left interlobar artery Figure 1a-c: Aneurysm in the left interlobar artery (initial imaging).
Figure 2d-f. Migratory aneurysm in the right main pulmonary artery (follow-up imaging); the last 3 images are follow-up imaging.
Discussion
This report emphasizes the diagnostic value of CT angiography and the importance of long-term follow-up for patients with Behçet vasculitis. Pulmonary artery aneurysms in Behçet vasculitis are rare conditions, but they carry a high risk of rupture and fatal hemoptysis. The migratory nature of pulmonary aneurysms, as observed in this case, is an exceptionally rare phenomenon. Literature review suggests that Behçet vasculitis typically presents with multiple pulmonary artery aneurysms rather than the resolution of one with subsequent development of another at a different location. This case aligns with previous reports where aneurysmal thrombosis led to spontaneous resolution, while new vascular lesions emerged due to ongoing systemic inflammation (6,7).
A study by Yildirim and coauthors and another study by Giannessi, emphasized the role of CT angiography in detecting and monitoring vascular involvement in Behçet disease, particularly in patients with evolving aneurysms. The unpredictable nature of vascular involvement necessitates serial imaging for disease monitoring (6). Furthermore, a meta-analysis highlighted the efficacy of immunosuppressive therapy in reducing aneurysm progression, underscoring the need for early initiation of treatment (8).
Management strategies for Behçet-related pulmonary aneurysms include high-dose corticosteroids and immunosuppressive agents, such as cyclophosphamide or azathioprine, with or without anticoagulation. Endovascular intervention or surgical repair is reserved for cases with a high risk of rupture. In this case, the patient’s refusal of surgical intervention underscores the need for individualized treatment plans, particularly in resource-limited settings.
Conclusion
This case highlights the migratory nature of pulmonary aneurysms in Behçet vasculitis, emphasizing the importance of early recognition, longitudinal imaging follow-up, and a multidisciplinary approach. Given the life-threatening potential of pulmonary aneurysms, timely diagnosis and intervention are crucial for optimizing patients’ outcomes.
References:
- Khan F, Gupta N, Khurana A, Zaheer S. Hughes-Stovin syndrome. Radiol Case Rep. 2017;12(3):550–3.
- Bowness J, Nair R, Anwar S, et al. Pulmonary artery aneurysms in Behçet’s syndrome. Clin Radiol. 2009;64(7):709–14.
- Seyahi E, Melikoglu M, Akman C, et al. Pulmonary artery involvement in Behçet’s disease. Clin Exp Rheumatol. 2008;26(4 Suppl 50): S27–33.
- Seyahi E. Behçet’s disease: How to diagnose and treat vascular involvement. Best Pract Res Clin Rheumatol. 2016;30(2):279–95.
- Emmi G, Silvestri E, Squatrito D, et al. Behçet’s syndrome as a model of thrombo-inflammation: From pathogenesis to treatment. Autoimmun Rev. 2022;21(11):103198.
- Yıldırım R, Oğuzman S, Dinler M, Bilge NŞY, Kaşifoğlu T. Scoping beyond pulmonary artery involvement; pulmonary involvement in Behcet’s disease; a retrospective analysis of 28 patients. Clin Rheumatol. 2023 Mar;42(3):849-853. doi: 10.1007/s10067-022-06423-5. Epub 2022 Nov 3. PMID: 36326947.
- Giannessi C, Smorchkova O, Cozzi D, et al. Behçet’s Disease: A Radiological Review of Vascular and Parenchymal Pulmonary Involvement. Diagnostics (Basel). 2022 Nov 19;12(11):2868. doi: 10.3390/diagnostics12112868.
- Atalar E, Erten S, Dogan I, Konak HE. Vascular Involvement in Behcet’s Disease: An Evaluation of 147 Cases and Literature Review. Sisli Etfal Hastan Tip Bul. 2023 Sep 29;57(3):380-386. doi: 10.14744/SEMB.2023.89083. PMID: 37900329; PMCID: PMC10600606.