Ognjanova Simjanovska V.1
1 University Clinic for Traumatology, Orthopedics, Anesthesiology, Resuscitation, Intensive Care and Emergency Center – Skopje, Department of Anesthesiology, Resuscitation and Intensive Care Medicine, “Ss Cyril and Methodius” University, Skopje, Faculty of Medicine
Abstract
Mass casualty events whether natural disasters, terrorist attacks, pandemics or large-scale accidents overwhelm healthcare systems, emergency departments and ICUs in minutes. High acuity situations require rapid coordination, strategic resource allocation and seamless inter-disciplinary collaboration. Anesthesiologists are uniquely positioned to play a central role in all phases of the response due to their expertise in airway management, hemodynamic stabilization, pharmacologic sedation and critical care. Their role extends beyond the OR to initial triage, emergency procedural support and ongoing management of ventilated and critically ill patients in the ICU. This article reviews current evidence and operational best practices to examine the role of anesthesiology in mass casualty events preparedness and response. Key areas of focus include disaster planning, ventilator triage, crisis standards of care, sedation protocols and ICU surge capacity. By highlighting the clinical, operational and ethical aspects of anesthesia management in mass casualty events, this article synthesizes current literature and best practices, emphasizing the anesthesiologists’ role in preparedness, immediate response and postoperative care during mass casualty events.
Key Words: mass casualty events, critical care, disaster preparedness, triage protocols.
Introduction
Mass casualty events present a challenge to the healthcare system requiring a coordinated, multidisciplinary response to optimize patients’ outcomes (1). As medical professionals, particularly anesthesiologists and critical care physicians, our role in the ER and ICU is pivotal in stabilizing and managing critically injured patients. These events arising from natural disasters, terrorist incidents, industrial catastrophes or pandemics necessitate meticulous preparedness and strategic anesthesia management to mitigate morbidity and mortality effectively (2).
Mass casualty events are defined as incidents in which the number and severity of casualties exceed the immediate capabilities of the local healthcare infrastructure (3). In the current era characterized by increasing geopolitical instability, climate change-related natural disaster and global pandemics, these events have become more frequent and complex. They necessitate a rapid and highly coordinated medical response (4). Hospitals particularly tertiary care centers must be prepared to receive and manage a sudden influx of critically ill or injured patients (5).
Anesthesiologists associated with perioperative care are playing critical roles beyond the confines of the operating theater. Their skill set uniquely qualifies them to manage airways, provide procedural sedation, conduct resuscitation and oversee critical care interventions under conditions of uncertainty and resources scarcity (6), from establishing emergent airways in chaotic emergency room settings to leading intensive care units overwhelmed with patients requiring mechanical ventilation and vasopressor support. In particular, the COVID-19 pandemic acted as a global mass casualty event revealing critical gaps in hospital preparedness and highlighting the role of anesthesiologists. During this time many were performing intubations and managing ventilators in unfamiliar and often high-risk environments. This unprecedented crisis underscored the need for a more integrated and systematic approach to anesthesia involvement in disaster response (7). Disaster preparedness is not solely about having equipment or protocols in place, it involves interdisciplinary collaboration, simulation-based training, real-time communication pathways and psychological readiness (8). Anesthesiology departments must be actively engaged in hospital disaster committees and scenario planning. As ICU capacities are rapidly overwhelmed by the influx of severely injured or unstable patients, anesthesiologists are tasked with delivering comprehensive care in high-pressure, resource-constrained environments (9).
Clinical Management during Mass Casualty Events
Mass casualty events are defined as large-scale incidents in which the number of injured overwhelms the capacity and resources of a local healthcare system. These scenarios are increasingly frequent due to geopolitical instability, climate-related disasters, pandemics and industrial accidents. The medical response to such events requires a well-orchestrated, interdisciplinary and adaptable approach that integrates emergency medicine, trauma surgery, anesthesia, nursing and critical care. This essay explores the elements of emergency and critical care during mass casualty events, triage, resuscitation, critical care strategies and the operational adjustments needed to sustain effective healthcare delivery under extreme situations.
Triage and Early Response
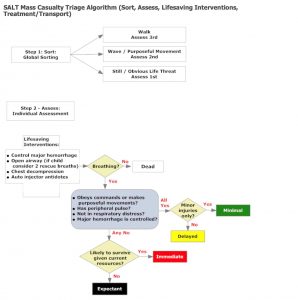
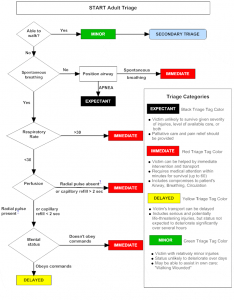
Triage is the foundation for efficient care delivery during a mass casualty event. The primary goal is to prioritize care based on injury severity, prognosis and available resources (10). Two of the most widely accepted systems are START (Simple Triage and Rapid Treatment) and SALT (Sort, Assess, Lifesaving Interventions, Treatment/Transport) (Figure 1, 2). These models stratify patients into categories such as Immediate, Delayed, Minor and Expectant (11). The Expectant category is ethically complex and acknowledges the need to allocate limited life-saving interventions where they are the most likely to succeed (12).
Initial triage occurs at the disaster site or at the emergency department entrance, often in chaotic conditions. Rapid assessment includes airway, breathing, circulation, disability (neurologic status) and exposure. Healthcare teams must be trained to make fast high-stakes decisions that can directly influence survival. Triage officers are typically experienced clinicians trained in disaster medicine or emergency care and their judgments must be supported by standardized protocols (13) .
Figure 1: Triage Decision-Making Process (14)
Figure 2: Triage Decision-Making Process (14)
Ethical Decision Making in Triage
Ethical issues did come into consideration during MCE triage situations where scarce resource limitation necessitates hard decisions (15). The Expectant category positions a patient as a victim unlikely to survive given available resources-evidence of one of those difficult decisions in triage. Again, guidelines from Disaster Ethics Protocols set down in past global crises can be used to administer such techniques in an ethical manner (16). Ethical frameworks were thus put in place for allocating scarce resources, such as ventilators, in the 2020 First Wave of COVID-19. Likewise, the events in 2020 from the Beirut blast threw into question the presence of clear triage protocols that allow for ethical management of the overburdened influx of patients. These principles may, for instance, include maximizing benefits, treating people equally, giving priority to instrumental value and giving priority to the worst off (16).
Airway and Respiratory Management
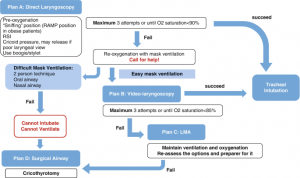
Airway compromise is a leading cause of preventable mortality in trauma and disaster settings. Early airway intervention is critical and must be executed with both speed and precision (figure 3). Rapid Sequence Intubation (RSI) remains the preferred method for securing airways in patients with depressed consciousness, facial trauma or respiratory failure (17). Induction agents such as ketamine (due to its sympathetic stimulation) or etomidate (for hemodynamic stability and neuroprotection) are commonly utilized in conjunction with neuromuscular blockers like succinylcholine or rocuronium. In environments where intubation is unsuccessful or not immediately possible, supraglottic airway devices (laryngeal mask airways) offer effective temporizing measures. Inhalational injuries, aspiration and thoracic trauma can complicate airway management and require multidisciplinary input including respiratory therapy and pulmonology (18). Mechanical ventilation, once established, must adhere to lung-protective principles especially in patients with acute respiratory distress syndrome (ARDS), a common complication in mass casualty events involving inhalation burns, sepsis, or blunt chest trauma. Low tidal volume ventilation (6mL/kg ideal body weight), appropriate positive end-expiratory pressure (PEEP) and plateau pressure monitoring help to prevent ventilator-induced lung injury.
Figure 3: Algorithm Airway Management in Mass Casualty Events (19)
Hemodynamic Resuscitation and Shock Management
Circulatory collapse from hemorrhagic shock, sepsis or cardiac trauma is another critical threat in mass casualty events patients. Damage control surgery is for patients with massive trauma or exsanguination focused on resuscitation and minimizing anesthesia time. The goal of damage control surgery is to control bleeding and contamination deferring definitive repair until the patient is stabilized (20). Damage control resuscitation is early hemorrhage control, permissive hypotension (in absence of traumatic brain injury) and balanced transfusion of blood products in a 1:1:1 ratio of red blood cells, plasma and platelets (21). This strategy aims to mitigate the “lethal triad” of coagulopathy, acidosis and hypothermia that drives poor trauma outcomes. In patients with traumatic brain injuries maintaining adequate cerebral perfusion pressure, minimizing intracranial pressure and avoiding hypoxia and hypercapnia are key anesthetic objectives. Sedation, controlled ventilation and osmotic agents are needed. Fluid resuscitation must be carefully managed to avoid exacerbating edema, compartment syndromes or dilutional coagulopathy. Balanced crystalloids such as Lactated Ringer are preferred over normal saline to reduce the risk of hyperchloremic acidosis. Vasopressors like norepinephrine and vasopressin may be necessary in patients with persistent hypotension despite adequate volume resuscitation. Invasive hemodynamic monitoring through arterial lines and central venous catheters, as well as the use of point-of-care ultrasound, assists in real-time decision-making regarding fluid responsiveness and cardiac function.
Critical Care and ICU Expansion
As the acute resuscitation phase transitions to critical care the focus shifts to organ support, prevention of secondary complications and eventual recovery. Intensive care units often reach capacity quickly during mass casualty events. Therefore, hospitals must have pre-planned surge strategies that allow perioperative areas such as post anesthesia care units, procedural suites and even operating rooms to be converted into intensive care units (22). Patients in the ICU frequently require prolonged mechanical ventilation, renal support, vasopressor therapy and complex nutritional management. In patients unresponsive to fluid resuscitation, vasopressors such as norepinephrine (first line) and vasopressin (as adjunct) are used to maintain perfusion pressure and prevent organ failure. Continuous renal replacement therapy is frequently needed in patients with acute kidney injury secondary to rhabdomyolysis, hypoperfusion or sepsis. For those with refractory hypoxemia or cardiac collapse, extracorporeal membrane oxygenation (ECMO) may be considered, although it is resource-intensive and requires highly specialized personnel. Neurocritical care is a parallel priority in patients with traumatic brain injuries, spinal cord injuries, or anoxic brain damage. The maintenance of cerebral perfusion pressure, prevention of intracranial hypertension and the judicious use of osmotic therapy are key components. Sedation protocols in the ICU are adapted to preserve neurologic examination and prevent delirium. Agents such as dexmedetomidine offer anxiolysis and light sedation without respiratory depression, while propofol and midazolam are reserved for deeper sedation when indicated.
Pain Control and Sedation
Pain and agitation in critically ill patients can lead to increased metabolic demand, sympathetic overdrive and worsened outcomes. Acute pain leads to elevated catecholamine levels, immunosuppression and impaired ventilation, all of which can worsen outcomes. A multimodal analgesic strategy is essential to reduce opioid consumption and minimize side effects. This includes the use of acetaminophen, NSAIDs (if renal function is intact), local anesthetics and regional techniques such as nerve blocks or epidurals when feasible. Sedation must be carefully titrated to balance comfort with the ability to conduct neurologic assessments. During mass casualty events the scarcity of agents may necessitate prioritization of long-acting or easily stored drugs. Providers must also remain vigilant for the development of ICU acquired delirium, necessitating regular sedation interruptions and cognitive assessments.
Preparedness, Training and Systems-Based Readiness
Effective disaster response hinges not just on individual competence but on institutional readiness. Hospitals must adopt an Incident Command System to establish a structured chain of commands, promote interagency collaboration and streamline communication. Pre-event planning should include hospital-wide simulation exercises that incorporate mass triage, patient flow management and mock casualties (23).
Clinical teams must receive ongoing education in trauma care, critical care and disaster ethics. Simulation-based training is particularly valuable, enabling teams to rehearse rare but high-impact scenarios in a controlled setting. Such training improves team coordination, leadership under pressure, and adherence to best practices (24).
Mass casualty events represent a test of a healthcare system’s resilience, preparedness and cohesion. Success in managing such events requires a well synchronized response that integrates rapid triage, advanced critical care, ethical resource allocation and continual training. While clinical skills are vital, it must be coupled with systems-level planning, real-time communication and flexibility in repurposing resources (24). Whether the casualties are from an earthquake, explosion or pandemic, the guiding principles remain constant: preserve life, alleviate suffering and maintain the integrity of the health system under duress. In such moments, the entire healthcare team like emergency physicians, surgeons, intensivists, anesthesiologists, nurses and support staff becomes a single organism functioning with one purpose, to restore order to chaos.
Discussion
In mass casualty events, taking care of seriously injured or critically ill patients is a huge challenge. Anesthesiologists play a key role in this response, both in the emergency room and in the intensive care unit (25). Their responsibilities range from rapid intubation and resuscitation to the provision of sedation, analgesia and long-term mechanical ventilation. These responsibilities are often carried out under pressure with limited resources and incomplete information, and experience and preparedness are essential for patients’ outcomes (26). In the emergency room anesthesiologists are frequently called upon to assist with airway management, hemodynamic stabilization and procedural sedation for trauma patients and critically ill patients. Their expertise in pharmacologic agents allows for efficient and safe interventions in unstable patients. Moreover, the anesthesiologists’ ability to work in high-stress environments, make quick decisions, and function in interdisciplinary teams makes them invaluable during the initial phases of disaster responses. In the ICU, anesthesiologists play a central role in managing ventilation strategies, sedative regimens, fluid resuscitation and vasopressor support. During mass casualty events ICU often exceed capacity requiring non-traditional spaces such as post anesthesia care units or operating rooms to be repurposed. Anesthesiologists are uniquely qualified for their ability to manage multiple critically ill patients simultaneously.
An overlooked aspect of anesthesiology involvement is participation in the hospital disaster planning and preparedness activities. Anesthesiologists should be involved in emergency planning and taking part in drills that simulate real-life crises with difficult decisions when resources are depleted. Ethical considerations such as allocation of resources pose serious moral dilemmas. In these situations, anesthesiologists may be asked to participate in or even lead triage teams that determine who receive potentially life-saving interventions (27). Having established guidelines with ethical principles and support by institutional leadership can help mitigate the moral burden on clinicians. This can help reduce the emotional and moral stress on healthcare workers making hard decisions in the middle of a disaster (28).
Conclusion
Mass casualty preparedness and anesthesia management demand a systematic, well-coordinated and multidisciplinary approach to optimize patients’ survival, reduce morbidity and ensure the effective utilization of scarce resources. In such high acuity and resource limited scenarios, anesthesiologists and intensivists serve as essential frontline providers. Their expertise in airway management, resuscitation, perioperative care, critical care pharmacology and mechanical ventilation uniquely equips them to manage both the acute and prolonged phases of patient care in the emergency room and intensive care unit. Beyond their clinical skillsets, anesthesiologists also contribute meaningfully to disaster planning, ethical decision making under crisis standards of care and systems level problem solving. Their role in simulation training, triage development and rapid response protocol implementation enhances institutional resilience and preparedness. An effective mass casualty response cannot succeed without strong interdisciplinary collaboration, frequent drills, logistical readiness and a clear delineation of roles. Integrating anesthesiology more deeply into institutional emergency protocols, command structures and preparedness committees ensures not only better outcomes during disasters but also a more adaptive and unified healthcare response.
References:
- Kelen GD, McCarthy ML. The science of surge. Acad Emerg Med. 2006;13(11):1089–1094.
- Christian MD, Sprung CL, King MA, et al. Triage: care of the critically ill and injured during pandemics and disasters: CHEST consensus statement. Chest. 2014;146(4):e61S–e74S.
- Hick JL, Hanfling D, Wynia MK, Pavia AT. Duty to plan: health care, crisis standards of care, and novel coronavirus SARS-CoV-2. NAM Perspectives. 2020.
- Ciottone GR. Disaster Medicine. 2nd ed. Elsevier; 2015.
- Devereaux AV, Dichter JR, Christian MD, et al. Definitive care for the critically ill during a disaster: a framework. Chest. 2008;133(5):1115–1123.
- Matava CT, Kovatsis PG, Lee JK, et al. Pediatric airway management in COVID-19 patients. Anesth Analg. 2020;131(1):61–73.
- Uppal V, Sondekoppam RV, Landau R, El-Boghdadly K, Narouze S. Neuraxial anaesthesia and peripheral nerve blocks during the COVID-19 pandemic. Reg Anesth Pain Med. 2020;45(7):581–588.
- Sprung CL, Zimmerman JL, Christian MD, et al. Recommendations for intensive care unit and hospital preparations for an influenza epidemic or mass disaster. Intensive Care Med. 2010;36(3):428–443.
- Thomas MJ, Sanford P. Operating rooms and PACUs as temporary ICUs. Anesthesiol Clin. 2020;38(4):785–794.
- del Carmen Cardós-Alonso, M., Otero-Varela, L., Redondo, M. et al.Extended reality training for mass casualty incidents: a systematic review on effectiveness and experience of medical first responders. Int J Emerg Med 17, 99 (2024).
- Lerner EB, Schwartz RB, Coule PL, et al. Mass casualty triage: an evaluation of the data and development of a proposed national guideline. Disaster Med Public Health Prep. 2008;2(S1):S25–S34.
- Persad G, Wertheimer A, Emanuel EJ. Principles for allocation of scarce medical interventions. Lancet. 2009;373(9661):423–431.
- Iserson KV. Triage in medicine, part I: concept, history, and types. Ann Emerg Med. 1992;19(3):268–272.
- Crisis Medicine. START, SALT, and RAMP: Triage in a Mass Casualty Event. Crisis Medicine. Published October 4, 2022. Accessed May 14, 2025.https://www.crisis-medicine.com/start-salt-and-ramp-triage-in-a-mass-casualty-event/
- Cuthbertson J, Penney G. Ethical Decision Making in Disaster and Emergency Management: A Systematic Review of the Literature. Prehospital and Disaster Medicine. 2023;38(5):622-627. doi:10.1017/S1049023X23006325.
- Ekmekci, P.E., Zhang, L. and Crawley, F.P. (2025) ‘Ethics Underpinning Data Policy in Crisis Situations’, Data Science Journal, (24), p. 4.
- Sakles JC, Laurin EG, Rantapaa AA, Panacek EA. Airway management in the emergency department. Emerg Med Clin North Am. 1998;16(1):27–48.
- Cook TM, Woodall N, Frerk C. Major complications of airway management in the UK. Br J Anaesth. 2011;106(5):617–631.
- Barak, M., Leiser, Y., Kluger, Y. (2019). Airway Management in Trauma Patients. In: Aseni, P., De Carlis, L., Mazzola, A., Grande, A.M. (eds) Operative Techniques and Recent Advances in Acute Care and Emergency Surgery. Springer, Cham.
- Rotondo MF, Schwab CW, McGonigal MD, et al. Damage control: an approach for improved survival in exsanguinating penetrating abdominal injury. J Trauma. 1993;35(3):375–382.
- Holcomb JB, del Junco DJ, Fox EE, et al. The Prospective, Observational, Multicenter, Major Trauma Transfusion (PROMMTT) Study. JAMA Surg. 2013;148(2):127–136.
- Curtis JR, Rubenfeld GD. Managing ICU triage during a pandemic crisis: the importance of process. Crit Care Med. 2020;38(6 Suppl):S1–S3.
- Gaba DM. Crisis resource management and teamwork training in anesthesia. Br J Anaesth. 2010;105(1):3–6.
- Ramaswamy V, Li J, Munoz R, et al. Simulation-based disaster preparedness training improves hospital staff’s response performance. Disaster Med Public Health Prep. 2021;15(3):353–359.
- Wax RS, Christian MD. Practical recommendations for critical care and anesthesiology teams caring for novel coronavirus patients. Can J Anaesth. 2020;67(5):568–576.
- Rosenbaum L. Facing COVID-19 in Italy—ethics, logistics, and therapeutics on the epidemic’s front line. N Engl J Med. 2020;382(20):1873–1875.
- Emanuel EJ, Persad G, Upshur R, et al. Fair allocation of scarce medical resources in the time of COVID-19. N Engl J Med. 2020;382(21):2049–2055.
- Truog RD, Mitchell C, Daley GQ. The toughest triage—allocating ventilators in a pandemic. N Engl J Med. 2020;382(21):1973–1975.