UDK: 616.366-089.819-06
Peneva E.1, Gjorgjioska S.1, Kocev Bundovska S.1,2
1Institute of Radiology, 1000 Skopje, Republic of North Macedonia
2Faculty of Medicine, “Ss Cyril and Methodius” University in Skopje, Republic of North Macedonia
Abstract
Acute cholecystitis is a condition which treatment usually involves surgery, and the most used is laparoscopic cholecystectomy. Bile leakage is a complication of laparoscopic cholecystectomy, often caused by injury to small aberrant bile ducts, such as the ducts of Luschka. We report a case of a 25-years-old female who was presented with abdominal pain five days after laparoscopic cholecystectomy. A CT scan and MRCP scan revealed a small bile collection in the gallbladder bed and the bile leakage was suspected. A laparoscopic revision was performed, during which a biliary collection was aspirated. Further exploration of the gallbladder fossa revealed an aberrant bile duct (duct of Luschka), smaller than 1mm, actively secreting bile. The duct was successfully closed, leading to resolution of the leakage. The ducts of Luschka are one of the most common causes of bile leakage after laparoscopic cholecystectomy. Generally, most of the diagnoses are determined post operatively as a result of the post-operative complications that arise. It is important to take into consideration the imaging reports whenever we have post cholecystectomy bile leakage.
Key Words: bile leakage; ducts of Luschka; laparoscopic cholecystectomy; magnetic resonance cholangiopancreatography.
Introduction
Acute cholecystitis is an inflammation involving the gallbladder. Most commonly the reason is blockage of the cystic duct which leads to accumulation of bile, chemical injury, inflammation, hydrops and secondary bacterial infection of the gall bladder. About 95% of the patients with acute cholecystitis have cholelithiasis, only 5% don’t have cholelithiasis. Usually the treatment involves surgery, the most commonly used is laparoscopic cholecystectomy which is a relatively safe procedure. The second most common complication that can arise is biliary tract leakage, which most often is associated with accessory ducts of Luschka or subvesical ducts that are an anatomic variation of the biliary ducts. Although they have important clinical impact, they can often be overlooked during routine imaging as the reason for the bile leakage. Radiological investigations that can be used are abdominal ultrasound (US), computed tomography (CT) scan and magnetic resonance cholangiopancreatography (MRCP) (1-5).
Case Report
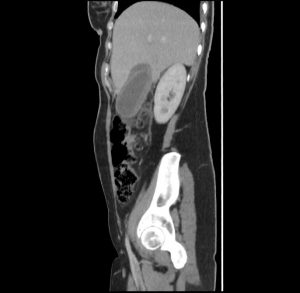
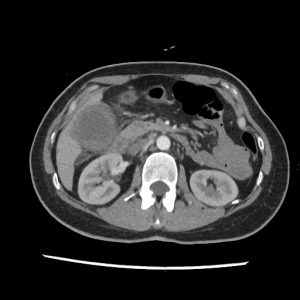
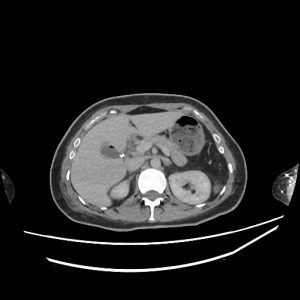
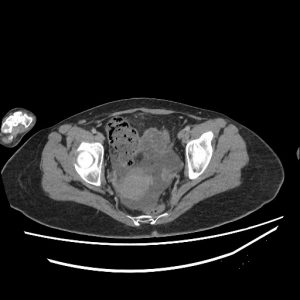
A 25-years-old female patient was presented to the emergency department with nausea, vomiting and pain under the right rib cage for 4 days. On clinical examination, the abdomen was soft, but tenderness was noted in the right upper quadrant. Laboratory results showed elevated white cells, counting 17.5 (normal range: 4.00-9.00 10/9L), elevated CRP 82.8 (normal range: under 6mg/L), also elevated total bilirubin 23 (normal range under 20.5umol/L) and direct bilirubin 9.1 (normal range: under 6.8umol/L). Accordingly, an emergency CT scan of the abdomen with intravenous contrast was performed next, where the cholecyst was noted to have a stratified and edematous wall and intraluminal denser contents with a sediment formed in the fundus. Also a suspicious mural defect was present in the proximal part of the posterior wall. Pericholecystic free fluid was present that extended subhepatic with stranding of the mesenteric adipose tissue. Loco regionally several enlarged lymph nodes were detected with a diameter of up to 10mm. Free fluid was also present in the small pelvis. The CT finding was in favor of acute perforating cholecystitis.
A decision for surgical treatment was made. The procedure involved laparoscopic retrograde cholecystectomy with removal of the gallbladder through a supraumbilical incision, peritoneal lavage was performed, and intraperitoneal drain was placed. The patient was discharged in good general condition.
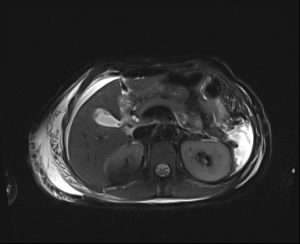
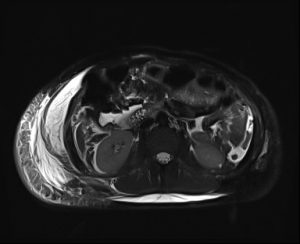
Five days after the operative treatment, the patient experienced severe abdominal pain accompanied by nausea and vomiting. The laboratory results showed elevated white cells count 11.1 (normal range: 4.00-9.00 10/9L), elevated CRP 67.3 (normal range: under 6mg/L), normal total bilirubin 14 (normal range under 20.5umol/L) and elevated direct bilirubin 10.2 (normal range: under 6.8umol/L). Control CT scan of the abdomen with intravenous contrast was performed, where in the region of the gall bladder a dense free liquid collection was observed, around which small free air inclusions were present, the clips of the cystic artery and ductus cysticus were also visible, and a smaller amount of free liquid was present in the pelvis.
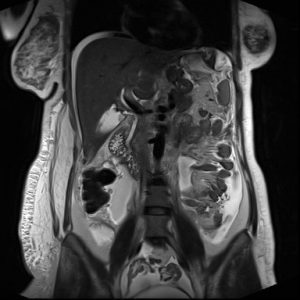
An MRCP was performed next, that showed intact common bile duct and intact cystic duct stump. Also, an area of fluid accumulation was noted in the subhepatic space, intraintestinal and in the small pelvis. Subcutaneous oedema in the right lateral abdominal wall was also noted, most likely post operatively.
An indication for postoperative laparoscopic revision was made where a larger biliary collection was found in the abdomen that was aspirated, and after a thorough exploration of the gall bladder bed, an aberrant bile duct smaller than 1mm was observed that is a Luschka subvesical duct, which secreted bile with an extremely small content. A biliary stasis was performed with a ligation of the aberrant Luschka duct using sutures and two intraperitoneal drains were placed for drainage. The postoperative course was in order. The control CT of the abdomen and pelvis after 2 weeks showed complete resorption of the free fluid in the abdomen and pelvis. In the region of the gall bladder fossa, several more air inclusions were observed, which would be in favor of a normal postoperative reaction. The patient was discharged for home treatment in good general condition with advice given for a hygiene-dietary regimen and antibiotic therapy according to the protocol for operated patients.
Discussion
The accessory ducts of Luschka, also called subvesical bile ducts are small ducts usually with a diameter of around 1 to 2mm, that drain sub segmental areas of the liver into the right hepatic duct (6,7). The overall prevalence in the general population is around 4% (6). Due to their small caliber and especially in a urgent setting of laparoscopic cholecystectomy, they can be overlooked, which would lead to post-operative complications like bile leakage (8,9). Generally, most of the diagnoses are determined post operatively as a result of the post-operative complications that arise (8). Imaging methods that can be used are US (ultrasound), CT (computed tomography), MRCP (magnetic resonance cholangiopancreatography) and ERCP (endoscopic retrograde cholangiopancreatography). However, they present a diagnostic difficulty and most often they are overlooked (6,8). US is usually the initial diagnostic method, with a sensitivity of around 70% for detection of intra-abdominal bile collections, however it isn’t very specific and is operator dependent (3,11-13). CT is more advanced method with a reported sensitivity of around 95% for detection of bile collection but cannot differentiate it from other fluid collections (6,10-13). ERCP is the most commonly used and is considered as the gold standard for the diagnosis of bile leakage after cholecystectomy. Its sensitivity is 95-100%. Also, it has high specificity of around 95%. With ERCP the sites of bile leakage can be evaluated with direct visualization of the contrast extravasation. However, this diagnostic procedure is invasive (9,12-14). MRCP is a non-invasive diagnostic procedure that can be used for assessing the anatomic structures of the biliary system with excellent detail. There are reported cases in literature, although uncommon when MRCP usually in combination with CT was successfully used for the diagnosis of bile leakage from Luschka ducts. Its sensitivity ranges from 67% to 100% and depends on many factors. Multidisciplinary approach is crucial for the fast detection of this complication after laparoscopic cholecystectomy and the radiologist should be aware of the diagnostic possibility of MRCP (6,10,11,15,16).
Conclusion
Imaging methods, especially CT and MRCP, play an important role in detecting and managing bile leaks after cholecystectomy. They help in identifying fluid collections and assess biliary anatomy and anatomic variations as the subvesical ducts of Luschka. It is important that the imaging reports take them into consideration whenever we have post cholecystectomy bile leakage, which will help in expediting the treatment of the patients.
References:
- Jones MW, Genova R, O’Rouke MC. Acute Cholecystitis. In: StatPearls. Treasure Island (FL): StatPearls Publishing; May 22, 2023
- Vitiello, A., Spagnuolo, M., Persico, et al. Biliary Leak from Ducts of Luschka: Systematic Review of the Literature. Surgeries 2024, 5, 63-72. doi:10.3390/surgeries5010008.
- Garcia S., Concepción AM., Wakoff C. “Bile Leak Due to Luschka Duct Injury After Laparoscopic Cholecystectomy: A Case Report.” Cureus vol. 14,8 e28427. 26 Aug. 2022, doi:10.7759/cureus.28427.
- Muleta J, Belayneh E, Haile K, et al. “A rare case of bile leak due to type 2 duct of Luschka injury post open cholecystectomy: a case report.” Journal of surgical case reports vol. 2024,3 rjae179. 21 Mar. 2024, doi:10.1093/jscr/rjae179.
- Bozer, A. “Hepatobiliary-Specific MRI Contrast Agent Detection of Subvesical Duct (Luschka’s) Injury Post-Laparoscopic Cholecystectomy: A Case Report”. Journal of the Belgian Society of Radiology, vol. 108, no. 1, 2024, p. 21, doi:10.5334/jbsr.3532.
- Lin, Y. H., Lin, C. W., Yin, W. Y. “Subvesical Duct Detected by Magnetic Resonance Cholangiopancreatography (MRCP) in a Patient with Bile Leak after Laparoscopic Cholecystectomy.” CRSLS: MIS case reports from SLS vol. 8,1 e2020.00074. 1 Apr. 2021, doi:10.4293/CRSLS.2020.00074.
- Parampalli U., Helme S., Asal G., et al. Accessory cystic duct identification in laparoscopic cholecystectomy, Grand Rounds Vol 8 pages 40–42, DOI: 10.1102/1470-5206.2008.0014.
- Selleslag, S., Vandeputte, M., Walgraeve, M.-S. “Unveiling the Hidden Culprit: A Case of Bile Leakage Post-Cholecystectomy Caused by a Luschka Duct”. Journal of the Belgian Society of Radiology, vol. 107, no. 1, 2023, p. 59, doi:10.5334/jbsr.3233.
- Gómez NA, Gutiérrez JO. Ducts of Luschka: A Review. Clin Surg. 2017; 2:1744.
- Carannante F., Mazzotta E., Miacci V., et al. Identification and management of subvesical bile duct leakage after laparoscopic cholecystectomy: A systematic review, Asian Journal of Surgery, Volume 46, Issue 10, 2023, Pages 4161-4168, doi:10.1016/j.asjsur.2023.04.031.
- Thomas S, Jahangir K. Noninvasive Imaging of the Biliary System Relevant to Percutaneous Interventions. Semin Intervent Radiol. 2016 Dec;33 (4):277-282. doi: 10.1055/s-0036-1592328.
- Walker AT, Shapiro AW, Brooks DC, et al. Bile duct disruption and biloma after laparoscopic cholecystectomy: imaging evaluation. AJR Am J Roentgenol. 1992;158(4):785–9. doi: 10.2214/ajr.158.4.1532111
- Yun SU, Cheon YK, Shim CS,et al. The outcome of endoscopic management of bile leakage after hepatobiliary surgery. Korean J Intern Med. 2017 Jan;32(1):79-84. doi: 10.3904/kjim.2015.165.
- Kim K. H., Kim T. N. Endoscopic management of bile leakage after cholecystectomy: a single-center experience for 12 years. The Korean journal of internal medicine vol. 32,1 (2017): 79-84. doi:10.3904/kjim.2015.165.
- Griffin N, Charles-Edwards G, Grant LA. Magnetic resonance cholangiopancreatography: the ABC of MRCP.Insights Imaging. 2012 Feb;3(1):11-21. doi: 10.1007/s13244-011-0129-9.
- Argirò, R.; Sensi, B.;Siragusa, L.; et al. Liver-Specific Contrast-Enhanced Magnetic Resonance Cholangio-Pancreatography (Ce-MRCP) in Non-Invasive Diagnosis of Iatrogenic Biliary Leakage. Diagnostics 2023, 13, 1681. Doi :10.3390/diagnostics1310168