UDK: 616-001-083.98
https://www.doi.org/10.55302/MJA2484166v
Vasilevska S1, Mojsova-Mijovska M1,2, Kavazovich A1, Trenchevska S2, Dimitrovski A2, Gavrilovska BrzanovA2
1 Faculty of Medical Sciences, “GoceDelchev” University, Shtip, Republic of North
Macedonia, Medical School – Second cycle studies – medical nurse specializing in
intensive care
2University Clinic for Traumatology, Orthopedics, Anesthesia and Intensive Care and Emergency Center, Clinical Center “Mother Theresa”, Faculty of Medicine, at “Ss. Cyril and Methodius” University, Skopje, Republic of North Macedonia
Abstract
Background: When a patient experiences more than two serious injuries that endanger their life or the function of essential organs, it is known as polytrauma. To lower the danger of death or long-term sequelae, this complicated medical issue necessitates immediate interdisciplinary treatment. Rapid evaluation of vital functions, patient’s stabilization, and provision of the required diagnostics for additional intervention, form the cornerstone of treatment.
Aim: The study aims to analyze the processes involved in caring for patients with polytrauma, from initial assessment and stabilization to secondary resuscitation, treatment and rehabilitation. It emphasizes the importance of an organized medical approach in reducing mortality, morbidity and disability among these patients.
Materials and methods: The study is a retrospective analysis of the total number of patients with polytrauma admitted and treated at University Clinic for Traumatology, Orthopedics, Anesthesia, Reanimation, Intensive Care and Emergency Center (UCTOARICEC), Clinical Center “Mother Theresa” at the Intensive Care Unit in Skopje. We included patients aged between 2 and 96 years, spanning a three-year period (2021–2023). We collected and processed data from patients’ admission records, age, gender, place of residence, diagnosis and outcomes, using documentation and statistics maintained at Clinic for Anesthesia, Reanimation, Intensive Care. We processed and analyzed the data using appropriate statistical methods, which included measures of central tendency, such as mean, median, and mode.
Results: According to the research conducted over the past three years, most of the polytraumatized patients were male, with the highest number of such patients admitted in 2021. We presented statistical analysis and data collection in tables and graphs, based on gender, place of residence, type and origin of injury and age.
Conclusion: Over the past few decades, there has been a significant increase in the number of polytrauma cases and multiple injuries. Today, polytrauma ranks third after malignancies and heart diseases. Modern approaches to treating polytrauma greatly benefit from algorithms, which help achieve better outcomes by minimizing omissions and errors and elevating the quality of healthcare to the highest level.
KeyWords: management; multiple injured patients; polytrauma.
Introduction
Traumatic injury is a preventable disease that has existed since the beginning of civilization. Humans have never been immune to injuries. There is substantial evidence showing that even the most primitive ancestors of modern humans were familiar with many fracture treatment techniques (1). About 150 years ago, primary amputation was the treatment for open fractures, which were synonymous with death due to hemorrhage or sepsis. The mortality rate for open fractures remained high (>50%) even in the 19thcentury, despite conditions that were considered ideal at the time. The prognosis of patients with fractures significantly improved with advances in understanding of bacterial contamination and infection transmission, thanks to Pasteur, Koch, Lister and Semmelweis. Additionally, the use of the Thomas splint with fixed traction prior to hospital transportation and proper wound management, as advocated by Pare and Larrey (surgeon of Napoleon), significantly improved patients’ outcomes. Greek medicine was the first to use the term “trauma”. Hippocrates and the medical schools of that time developed a symptomatic approach to trauma. An external force can inflict an injury on the human body, ranging in intensity from minor to severe, as defined by the medical term trauma. Over time, the causes of trauma have changed, but its importance and impact on individuals and society remain significant (2).
Trauma occurs suddenly and without warning, most often affecting the young and productive population. The three most common mechanisms of major trauma are motor vehicle accidents, firearms and falls. Trauma is a leading cause of mortality and disability worldwide, representing a significant public health issue. Trauma mortality has a trimodal distribution: immediate death, early death and late death (3). Immediate deaths occur due to massive injuries like ruptured organs, while early deaths often result from conditions such as hemorrhagic shock. Late deaths, often from sepsis or multiple organ failure, can happen days or weeks after the injury. The “classic” trimodal distribution is associated with blunt trauma, while a bimodal distribution (early or immediate deaths) is characteristic of penetrating injuries (4).
More than half of all traffic-related deaths occur among vulnerable road users: pedestrians, cyclists and motorcyclists. Injuries sustained in traffic accidents are among the most severe, with high mortality rates on the site or later due to the injuries. However, 50% of fatalities occur at the site of the accident or within minutes. This is known as immediate death (immediate killing trauma), caused by factors such as rupture of the heart, aorta or major blood vessels, brain stem laceration, or severe cerebral hemorrhage. Of polytraumas, 30% can be classified as early deaths, occurring within hours due to tension pneumothorax, hemorrhagic shock, rupture of the liver or spleen, hypoxemia, compromised airways or brain injuries. During this period, surgical interventions are lifesaving, referred to as “damage control” in the “golden hour.” Effective resuscitation is crucial for the outcome. Out of all polytraumas, 20% can be classified as late death, occurring in the following days or weeks due to sepsis, respiratory issues, heart failure or acute multiple organ failure (MOF) (5,6).
The mechanisms of injury are classified into blunt, penetrating and thermal injuries. The severity of penetrating trauma is directly linked to the kinetic energy of the projectile at impact and the elasticity of the injured tissue. Projectiles cause a primary cavity due to crushing injury and a temporary cavity resulting from the blast effect on surrounding tissues. Blunt injuries distribute energy across a larger area compared to typical penetrating injuries, often resulting in multiple simultaneous injuries across different body parts. These injuries are more complex and challenging to treat. Thermal or inhalation injuries account for over 75,000 cases requiring hospital care annually, with a morbidity rate of 10% (7).
Patients with severe burns may initially appear stable upon admission, but within 24 hours can become critically endangered due to respiratory and circulatory failure. Treatment depends on the severity of the burns and the extent of inhalation injury (8).
The principles of care for patients with multiple traumas include simultaneous assessment and resuscitation, a thorough physical examination, diagnostic evaluations, and clear prioritization of life-saving surgical interventions. A well-organized trauma service can significantly reduce trauma-related mortality and morbidity by integrating pre-hospital care systems with trauma centers for definitive patient’s treatment (9).
Polytrauma is a medical term describing the condition of a person who has suffered multiple traumatic injuries affecting different parts of the body and organ systems. It is defined by the severity, location of injuries and the patient’s physiological parameters. Polytrauma typically involves at least two body systems, where one injury is life-threatening, such as damage to two body cavities alongside fractures of long bones.
According to classification in practical medicine, polytrauma is generally divided into three degrees:
- Grade I – Relatively mild injury without traumatic or hemorrhagic shock (with timely treatment, the outcome is favorable).
- Grade II – Moderate injuries with the development of traumatic shock (requiring long-term rehabilitation focused on stabilizing negative outcomes).
- Grade III – Fatal, extremely severe injuries leading to irreversible and rapid changes in life-supporting systems, with the possibility of saving life measured in minutes.
Clinical manifestations depend on the location, severity and systemic response to the traumatic factor (1).
The aim of our evaluation was to analyze and evaluate the critical care challenges associated with managing polytrauma patients in the intensive care unit (ICU), focusing on early assessment, stabilization, secondary resuscitation and rehabilitation to reduce mortality, morbidity and long-term disability rates.
Material and Methods
The study is a retrospective analysis of polytrauma patients admitted and treated at the University Clinic for Traumatology, Orthopedics, Anesthesia and Intensive Care and Emergency Center, Clinical Center “Mother Theresa”, at “Ss. Cyril and Methodius” University, Skopje, Republic of North Macedonia, in the Intensive Care Unit (ICU). The analysis spans a three-year period (2021–2023) and includes patients with injuries caused by unknown trauma, traffic accidents, gunshot wounds and sharp objects.
Inclusion Criteria: patients aged between 2 and 96 years, patients admitted to the Intensive Care Unit with documented polytrauma and patients with complete patients’ admission records with demographic data (age, gender, place of residence), diagnosis and outcomes.
The data were collected from the patient admission records and analyzed using documentation and statistics maintained at the Clinic for Anesthesia, Reanimation and Intensive Care. The data processing involved appropriate statistical methods, including measures of central tendency such as mean, median and mode.
Results
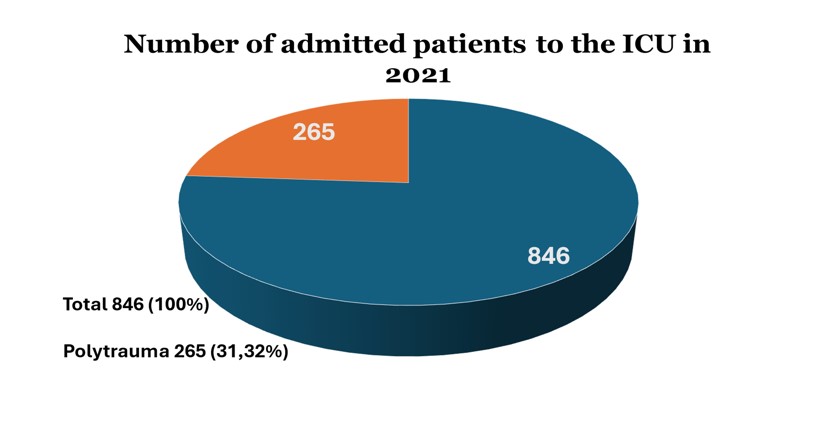
In 2021, the ICU of UCTOARICEC, Skopje, 846 patients were admitted during the study period, out of which 265 (31.32%) were polytrauma cases from unknown causes, traffic accidents, gunshot wounds and sharp object injuries (Graphic 1). Out of these, 151 (56.98%) required mechanical ventilation, while 114 (43.02%) were placed on oxygen masks. A total of 173 (65.28%) patients were discharged, 79 (29.81%) died, and 13 (4.91%) were transferred to other cities or countries. Among the deceased, 27 (34.18%) were victims of traffic accidents (Table 1).
Graphic 1. Graphical presentation of patients admitted to ICU in 2021.
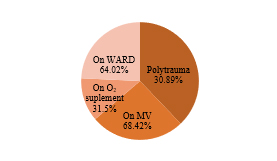
Out of the 738 patients hospitalized to the intensive care unit in 2022, 228 (30.89%) had polytrauma. Out of these, 72 (31.58%) were on oxygen masks, and 156 (68.42%) were on mechanical ventilation. Thirteen (5.70%) patients were sent to different cities or countries, 69 (30.26%) patients died, and 146 (64.04%) patients were discharged. 24 (34.78%) of the dead were involved in road accidents.
Graphic 2.Graphical representation of patients admitted to ICU in 2022.
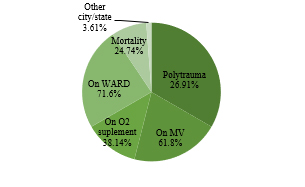
Out of the 721 patients hospitalized to the ICU in 2023, 194 (26.91%) had polytrauma. 120 (61.86%) of these were on mechanical ventilation, while 74 (38.14%) were using oxygen masks. Out of the patients, 139 (71.65%) were sent home, 48 (24.74%) passed away, and 7 (3.61%) were moved to another city or country. Twenty of the dead (41.67%) were involved in automobile accidents.
Graphic 3. Graphical representation of patients admitted to ICU in 2023.
ICU admissions declined over the three years (846 in 2021, 738 in 2022, 721 in 2023), reflecting either improved prevention or reduced trauma incidence. Polytrauma cases showed a downward trend (31.32% in 2021, 30.89% in 2022, and 26.91% in 2023). The percentage of polytrauma patients requiring mechanical ventilation increased slightly in 2022 (68.42%) compared to 2021 (56.98%) but decreased to 61.86% in 2023. Conversely, the use of oxygen masks decreased slightly over the three years, suggesting either a shift in treatment practices or case severity trends. Discharge rates improved significantly in 2023 (71.65%) compared to 2021 (65.28%) and 2022 (64.04%). Mortality rates declined notably from 29.81% in 2021 to 24.74% in 2023. Among deceased patients, the percentage of deaths due to traffic accidents fluctuated: 34.18% in 2021, 34.78% in 2022, 41.67% in 2023.
Table 1. Summarized a three-year comparison of ICU admissions.
| Year | Total ICU Admissions | Polytrauma Cases | Mechanical Ventilation | Oxygen Mask | Discharged | Mortality | Transfers |
| 2021 | 846 | 265 (31.32%) | 151 (56.98%) | 114 (43.02%) | 173 (65.28%) | 79 (29.81%) | 13 (4.91%) |
| 2022 | 738 | 228 (30.89%) | 156 (68.42%) | 72 (31.58%) | 146 (64.04%) | 69 (30.26%) | 13 (5.70%) |
| 2023 | 721 | 194 (26.91%) | 120 (61.86%) | 74 (38.14%) | 139 (71.65%) | 48 (24.74%) | 7 (3.61%) |
Discussion
This retrospective study analyzed polytrauma patients admitted to the ICU at UCTOARICEC, Clinical Center “Mother Teresa,” Skopje, from 2021 to 2023. A total of 265 (31.32%) polytrauma patients were admitted in 2021, 228 (30.89%) in 2022, and 194 (26.91%) in 2023, representing a significant portion of the ICU admissions during these years. These patients primarily sustained injuries resulting from traffic accidents, firearm injuries and sharp object injuries, with a smaller percentage having undetermined or unknown mechanisms of injury. This reflects the varied nature of polytrauma cases in our region and the diverse etiologies contributing to the burden of severe injuries.
The demographic breakdown revealed that most of the polytrauma patients were male (62%), consistent with global trends that show a higher incidence of trauma in males. The most affected age groups were individuals over 60 years and young adults aged 20-40 years, both of whom are at higher risk for severe injury due to factors such as reduced physical resilience in the elderly and risky behavior in younger adults (11,12). Notably, many patients were from regions outside the capital, Skopje, suggesting potential disparities in trauma care access and transport time, particularly for patients residing in rural areas. This highlights the need for strengthening pre-hospital and regional trauma care systems to reduce delays in care for patients in more distant locations (13).
Regarding clinical outcomes, mechanical ventilation was required for 151 (56.98%) patients in 2021, 156 (68.42%) in 2022, and 120 (61.86%) in 2023. The increased reliance on mechanical ventilation over the years reflects the growing severity and complexity of the polytrauma cases admitted to the ICU, underscoring the crucial role of advanced respiratory support in trauma management. The use of oxygen masks also remained significant, with 114 (43.02%) patients in 2021, 72 (31.58%) in 2022, and 74 (38.14%) in 2023 requiring supplemental oxygen. This highlights the varied clinical presentation and the necessity for tailored respiratory interventions depending on the patient’s condition (14,15).
Mortality rates in our study were notably high, with 79 (29.81%) deaths in 2021, 69 (30.26%) in 2022, and 48 (24.74%) in 2023. These figures are in line with global trauma mortality rates, though the proportion of trauma-related fatalities remained a significant concern [6]. Traffic accidents were the leading cause of death, accounting for 34.18% of the deaths in 2021, 34.78% in 2022, and 41.67% in 2023. This trend mirrors the broader global context where road traffic injuries remain the leading cause of trauma-related death, particularly in low- and middle-income countries (LMICs) like Republic of North Macedonia. In 2023, Republic of North Macedonia reported 127 fatalities due to traffic accidents, marking a 2.41% increase from the previous year. This reinforces the critical need for public health interventions aimed at improving road safety and reducing the burden of road traffic accidents. The findings align with broader regional and global trends in trauma care. Worldwide, approximately 1.35 million people die annually due to road traffic accidents, with Europe accounting for over 20,000 fatalities each year. In some countries, like Germany and Sweden, road safety measures have led to significantly lower fatalities, with Germany reporting 34 deaths per million people and Sweden – 22 per million. However, in Southern and Eastern Europe, including Republic of North Macedonia, the rates are higher, indicating a persistent gap in road safety compared to Western and Northern Europe. These disparities underscore the need for urgent interventions to improve road infrastructure and safety standards across the region (9,10,16).
Furthermore, raising public awareness regarding the dangers of alcohol consumption, distracted driving (e.g., mobile phone use), and speeding is crucial for improving road safety. Education campaigns targeting young drivers, stricter enforcement of traffic laws, and the implementation of advanced vehicle technologies such as collision avoidance systems can significantly reduce the risk of accidents (17).
The high incidence of polytrauma in our study highlights the need for continuous improvements in trauma care systems, from pre-hospital care through rehabilitation. Polytrauma patients often are presented with complex, multi-system injuries that require multidisciplinary management, including surgery, intensive monitoring and respiratory support. The role of ICU staff in managing these cases is critical, and ongoing training for healthcare professionals is essential to maintaining high standards of care. Furthermore, the development of robust rehabilitation systems is vital for improving long-term outcomes for trauma survivors (18-21).
Beyond the direct medical costs, non-fatal injuries impose a substantial economic burden on society due to lost productivity, long-term care needs and rehabilitation expenses. Developing more efficient trauma systems, improving patients’ outcomes through early intervention and investing in long-term rehabilitation services are crucial steps toward reducing both the human and economic costs of trauma (22,23).
Trauma management, particularly for polytrauma patients, requires a well-coordinated and multidisciplinary approach to effectively address the various aspects of patients’ care. A timely and accurate assessment, using tools such as the Rapid Trauma Assessment (RTA) or the Advanced Trauma Life Support (ATLS) guidelines, is crucial for identifying life-threatening injuries and stabilizing patients. Prompt intervention in pre-hospital setting and timely transport to specialized trauma centers have been shown to reduce mortality rates in polytrauma patients (20-23).
Once in the hospital, trauma care should follow established protocols to address airway management, hemorrhage control and prevention of shock, with close monitoring for signs of organ failure or complications such as infections. The use of modern technology, such as point-of-care ultrasound (POCUS) and CT imaging, helps in the rapid assessment and decision-making process, ensuring patients receive the most appropriate treatment quickly (24). In the ICU setting, adequate respiratory support and fluid management are critical components of trauma care, particularly in polytrauma cases that require mechanical ventilation and intensive monitoring (20).
Moreover, improving rehabilitation and long-term trauma care is essential to reducing the long-term disability burden. Early rehabilitation, multidisciplinary care, and addressing both the physical and psychological aspects of recovery can significantly enhance outcomes for patients, reduce the societal burden and improve quality of life post-trauma (25).
Conclusion
In conclusion, the findings of this study highlight the urgent need for a comprehensive, multi-sectoral approach to trauma care in the Republic of North Macedonia. Addressing the challenges of trauma care requires systemic improvements, including the development of infrastructure, better training for healthcare professionals, and enhanced public awareness on road safety and safe driving practices. These efforts should be coupled with strengthening healthcare systems to manage the growing burden of polytrauma. Strengthening trauma care protocols, from pre-hospital to rehabilitation, is essential for managing polytrauma cases effectively and ensuring that patients receive the necessary intensive care. Furthermore, addressing road safety, increasing public education will be crucial steps in reducing traffic-related injuries. The combined efforts of healthcare systems, governmental bodies, and society as a whole can lead to better survival rates and improved recovery for polytrauma patients, making a substantial impact on public health.
References:
- Saveski, J, et al. Special Surgery. Trauma of the Locomotor System, Volume I, University “St. Cyril and Methodius” – Faculty of Medicine, 2013, Skopje.
- Todorov, I., et al. Clinical Traumatology. University “St. Cyril and Methodius” – Faculty of Medicine, 2000, Skopje.
- Trunkey DD, Blaisdell FW: American College of Surgeons. Care of the surgical patient: epidemiology of trauma. Sci Am 1997; 1:4.
- Demetriades D, Kimbrell B, Salim A, Velmahos G, Rhee P, Preston C, Gruzinski G, Chan L. Trauma deaths in a mature urban trauma system: is “trimodal” distribution a valid concept? J Am Coll Surg. 2005 Sep;201(3):343-8. doi: 10.1016/j.jamcollsurg.2005.05.003. PMID: 16125066.
- Giannoudi M, Harwood P. Damage control resuscitation: lessons learned. Eur J Trauma Emerg Surg. 2016 Jun;42(3):273-82.
- Kaafarani HMA, Velmahos GC. Damage Control Resuscitation In Trauma. Scandinavian Journal of Surgery. 2014;103(2):81-88.
- Herndon DB (ed): Total Burn Care.2nd ed. Philadelphia, WB Saunders, 2001.
- Otterness K, Ahn C. Emergency department management of smoke inhalation injury in adults. Emerg Med Pract. 2018; Mar;20(3):1-24.
- The World Health Organization. Guidelines for essential trauma care. WHO 2017; https://www.who.int/ (accessed December 2024 ).
- European Union. https://road-safety.transport.ec.europa.eu/index_en (assesses December 2024 ).
- Honkanen R, Koivumaa-Honkanen H, Smith G. Males as a high-risk group for trauma: the Finnish experience. J Trauma. 1990 Feb;30(2):155-62.
- Baker C.C. et all.: Epidemiology of Traum deaths, The Journal of Surgery, vol./140, 144-149, 1980.
- Jarman MP, Castillo RC, Carlini AR, Kodadek LM, Haider AH. Rural risk: Geographic disparities in trauma mortality. Surgery. 2016 Dec;160(6):1551-1559.
- Flower L, Martin D. Management of hypoxaemia in the critically ill patient. Br J Hosp Med (Lond). 2020 Jan 2;81(1):1-10.
- Champion HR, Sacco W, Carnazzo AJ, Copes W, Fouty WJ. Trauma Score. Crit Care Med, 1981; 9:672-676.
- Charlton R, Smith G. How to reduce the toll of road traffic accidents. J R Soc Med. 2003 Oct; 96(10):475-6.
- Riuttanen, A., Jäntti, S.J. & Mattila, V.M. Alcohol use in severely injured trauma patients. Sci Rep 2020;10-17891.
- Boyd C.R.,Tolson M.A., Copes W.S.:Evaluating Trauma Care: The TRISS Method. Trauma Score and Injury Severity Score. J trauma 1987; 27:370-378.
- Nast-Kolb D., Jochum M.,Waydhas C., Schweiberer L.: Die KlinischeWertigkeitbiohemischerFaktorenbeim Polytrauma. Hefte Unfallheilkd 1991; 215:1-162.
- Committee on Trauma. American College of Surgeons: Advanced Trauma Life Support Manual: Course Overview. Chicago, American College of Surgeons 2002; :5.
- Committee on Trauma: Advanced Trauma Life Support Program for Doctors. Chicago, American College of Surgeons, 1997.
- Hubble MW, Hubble JP: Principles of Advanced Trauma Care. Albany, NY, Delmar, 2002.
- American College of Surgeons Advanced Trauma Life Support (ATLS) for Doctors faculty manual. Chicago, IL, American College of Surgeons 2004: 131.
- Brzanov N, Labacevski N, Antovik S, Trpevski S, OgnjenovicLj, Gavrilovska –Brzanov A. Implementation of focused assessment with ultrasonography in trauma patients in university surgical emergency department. MJA 2023;7(3):52-65.
- Goddard SD, Jarman MP, Hashmi ZG. Societal Burden of Trauma and Disparities in Trauma Care. Surg Clin North Am. 2024 Apr;104(2):255-26