UDK: 616-073.756.8:004
Chabukovska Radulovska J1,2
1 University Clinic for Surgical Disease “St. Naum Ohridski“, Skopje
2 Faculty of Medical Sciences, “Goce Delchev” University, Shtip.
Abstract
New medical CT technologies and devices have undoubtedly made great improvements in the diagnosis and treatment of human diseases. Simultaneously, inappropriate, or unqualified use of these technologies and medical equipment can cause unnecessary or unintended exposures and potential health hazards for the patients and medical personnel. These risks can be largely controlled, and benefits can be maximized by choosing appropriate procedures and methods to reduce patients’ exposure without reducing clinical efficacy. In the last few years, there has been an increased number of CT examinations in medical clinical practice which represents a large part of the collective dose of radiation from diagnostic examinations. At the same time average annual per capita radiation dose for diagnostic purposes is also increasing which contributed to growing the concern about radiation hazards among the population. Due to the increasing concern about the potential dangers of CT radiation, many strategies have been developed to reduce and optimize CT dose in order to maximize the benefit-risk ratio of CT examinations. Lifetime risks of CT examinations, the cumulative dose of CT radiation per capita, is very important especially in the young population who have higher radio-sensitivity and expectancy of longer life than the old ones. In this presentation, the currently available strategies for optimized CT protocols and reducing the CT dose are presented, which can lead the appropriate utilization of CT in diagnostic manner through good medical practices which can contribute to adequate radiation protection on patients.
Key Words: Computed tomography, optimization, radiation dose.
Introduction
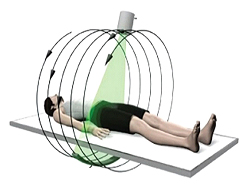
Modern medical CT technologies and devices have undoubtedly made great improvements in the diagnosis and treatment of human diseases. Simultaneously, inappropriate, or unqualified use of these technologies and medical equipment can cause unnecessary or unintended radiation exposures and potential health hazards for the patients and medical personnel. These risks can be largely controlled, and the benefits can be maximized, by choosing appropriate procedures and methods to reduce patients’ radiation exposure without reducing clinical efficacy (1). With the increased utilization of CT, the average annual per capita radiation dose for diagnostic purposes is also increasing. It raises concerns about radiation hazards among the population. In addition to that is the fact that the effective dose per capita has doubled in the last 10 years. Although the utility of modern diagnostic procedures is considerable, and the individual risk associated with radiation exposure from medical examinations is still generally low, the increasing number of examination with ionizing radiation and the number of exposed persons who have multiple examinations annually, is general public health issue, taking into account the fact that more than two-thirds of the radiation for diagnostic purposes are attributed to the computed tomography (head, chest, abdomen, pelvis) Figure 1.

Figure1.
For those reasons, CT is the primary focus of attention. Modalities such as fluoroscopy, angiography, interventional radiological procedures are also in the center because of the radiation doses. With the rise of the number of CT examinations, there is also growing concern about the danger of increased radiation from performing a greater number of examinations, at the same patients several times per year (2). For this reason, in recent decades much attention has been given to the optimization of the dose on CT examinations by radiologists, technologists and medical physicists. With the purpose to ensure the quality and safety in radiology, it is mandatory to systematically monitor and analyze the data concerning the dose from the radiological examinations, as well as monitoring of the images’ quality. New strategies for reducing the radiation dose during radiological diagnostic procedures are continuously being developed and radiologists have a key role in these dose management activities.
Most of the strategies to reduce CT dose are focused on the choice of the CT scan as an appropriate diagnostic test, limiting the examination to the anatomic area which is required, and optimizing the parameters of scanning (especially in pediatric patients). Only by applying optimized technical parameters radiation exposure could be reduced by up to 65%.
In the process of the dose optimization, multiphase examinations that include series without i.v. contrast and post contrast series (arterial, venous late series) should be considered especially in cases where one or fewer phases in the examination are sufficient. Multiphase CT studies (repeated scans before and after contrast injection) are potentially very important source of medically unnecessary radiation due to the dose multiplier effect of dose in the additional phases. Despite the facts that high levels of exposure to ionizing radiation increase the risk of cancer, the data for lower doses of radiation obtained in sequences or from multiple examinations are less clear and still controversial (3). Because of insufficient clarity surrounding this issue, the American College of Radiology, Health Physics Society, IAEA and other concerned organizations, have embraced the ALARA principle. This principle dictates that physicians should strive to reduce radiation exposure to the lowest achievable levels, focusing on what is medically necessary.
Regarding multiphase examinations, the American College of Radiology recognizing the need for guidelines, in 1993 developed the ACR Evidence-Based Appropriateness Criteria, that describe scanning protocols with specific phase selections for various clinical conditions (4). In 2014, ESR nominated experienced radiologists to develop European guidelines for imaging referrals according to eligibility criteria of the American College of Radiology. These guidelines are integrated into the ESR iGuide platform. Current international requirements linked to the medical use of ionizing radiation also take a part in International Basic Safety Standards (IAEA Safety Standards Series No. GSP Part 3) (5).
Regarding the improvement in medical clinical practice, establishing and maintaining a culture of radiation safety in health care, the three fundamental principles of radiation protection are important: Justification, Optimization, and Dose limit (6).
While quantifying the lifetime risks related to CT examinations involves uncertainties, it’s crucial to minimize the cumulative dose of CT radiation per person. This is particularly critical for younger individuals, given their heightened radiosensitivity and longer life expectancy compared to the older population (7).
CT Dose Parameters and Radiation Dose
Patient’s radiation exposure associated with CT is assessed using 3 main metrics:
1. Volume CT dose index (CTDI) vol.- represents the output dose of radiation from the scanner,
2. The dose length product (DLP) – represents the dose from the total scan and is derived from the CTDI volume including a scan length component,
3. The effective dose (ED) which measures the equivalent dose to the whole body with the same risk of biological effect. ED expressed as millisieverts (mSv), is formulated as a sum of absorbed doses of individual organs, weighted for their sensitivity to radiation.
Scan length (L) (Depends on patient height). Figure 2.
DLP = CTDI x L
DLPtotal = DLPseries х No (series)
Figure 2.
Parameters that Affects Radiation Dose and Images’ Quality in CT
Factors which directly affect the dose and image quality in CT include quality reference tube current, quality reference image noise, tube voltage, quality reference contrast to noise ratio, beam dimensions (width, height, z length), rescanning, reconstruction kernel, and iterative reconstruction algorithms (8).
Why the dose is so important?
The importance of radiation doses derives from the basic concepts of radiation and the evidence linking radiation exposure for medical purposes to the risk of developing cancer. Deterministic effects of radiation or so-called tissue reactions, such as skin erythema and hair loss, which result from cell death or radiation-induced damage, are in contrast with stochastic harmful effects on the population, such as cancer, which result from mutations. At the same time, the concepts of risk and dose were opposed. Certain radiobiological studies also indicate an increased risk for stochastic effects in pediatric and young adult population, compared to older adults for the same radiation exposure. Given that expression of stochastic damage takes many decades to become apparent, we may be just at the threshold of an increasing MDCT-induced cancer rate (9).
With the increased use of CT in recent years, there has been growing concern about the stochastic risks of radiation and safety in patient care.
Although CT accounts for only 17% of imaging studies obtained, statistics show that it is responsible for nearly half of the collective effective dose from medical procedures in the United States (Mettler et al. 2009) (10). Risk projection models for radiation-induced carcinogenesis predict that in a few decades, 1.5–2% of all cancers in the United States may be attributable to CT use (Brenner and Hall 2007). Although diagnostic CT examinations are generally performed for assumed clinical indication in which the net benefit to the individual patient outweighs the theoretically increased risk of radiation, induced malignancy growth in the use of CT exams, generally increases the likelihood of stochastic harmful effects on the population (expression of a cancerous disease). Because of this potential radiation risk from the increased use of CT, it is especially important that CT doses are kept as low as reasonably possible (10).
How to reduce the dose?
In order to reduce the radiation dose, the first step is to consider the clinical indication and justification of a particular CT examination. The process of dose optimization often involves multiple stakeholders: referring physician, radiologists, CT technologists, medical physicists and patients.
To comply with the “as far as reasonably practicable” principle, appropriate strategies to optimize CT examinations should also be developed (11).
CT equipment manufacturers are also striving to develop new techniques to reduce radiation dose while maintaining or improving image quality. Part of them are new types of detectors, automatic exposure control (AEC) systems and iterative reconstruction (IR) algorithms, as part of the most modern techniques for radiation dose optimization in CT.
An optimization approach to minimize the absorbed dose in patients undergoing a CT examination, at the same time, means maintaining a certain image quality of the diagnostic image, suitable for establishing a diagnosis, taking into account correlation with the image quality.
Regarding that, our practical goal is to find an optimization approach to minimize the absorbed dose in patients undergoing CT examination, while maintaining a certain quality of the diagnostic image.
CT scanners differ in their features both depending on the generation of the scanner and between different manufacturers type.
At the same time, the different indications require appropriate protocols that are in accordance with the clinical question. However, an essential primary step before any CT scan is to justify the medical need for the CT scanning. Radiologists influence the patient’s radiation dose by selecting imaging protocols and targeting body-specific and disease-specific protocols that can minimize dose. The goal when choosing protocols is not to create an image of the highest technical quality, but to generate a diagnostic image that enables the diagnosis of pathological changes, using the lowest possible dose.
That’s why strategies to reduce exposure to medical radiation largely have two primary goals:
1. Achieving greater awareness of the significance of medical radiation exposure.
2. Using new technology to obtain high-quality images from inherently noisier data.
According to that, CT dose reduction are a combination of different approaches or strategies.
These include Justification of CT diagnostic procedure; Optimization of scanning protocols and appropriate adjustments according to age or weight; Reduction of unnecessary examinations; Development of appropriate exposure protocols by manufacturers; Sufficient training and education for radiologists and radiologic technologists.
Dose Optimization
Optimization is the process of maintaining diagnostic image quality while minimizing the dose of ionizing radiation required to capture an image.
Optimization of CT radiation dose is an important issue that should be pursued first, starting with the choice of CT equipment and the proper training of the radiologists, radiologic technologists, and medical physicists.
To optimize CT examination protocols, an understanding of CT scan parameters and their effect on image quality is fundamental. There is also a need for standardization of CT diagnostic reference levels (DRLs) in accordance with the recommendations of the International Commission on Radiation Protection to reduce dose variations and facilitate comparison of doses (12). The same can be done by adopting international DRLs or making a DRL on the national level.
How to achieve an optimized dose?
The optimization of the radiation dose can be achieved by: Setting appropriate technical parameters; Optimizing the protocol according to the clinical question; Focusing on the training of professionals who are directly involved in the process of CT imaging and diagnosing changes, such as radiologists, technologists and medical physicists.
The best way to achieve dose optimization is to understand all the factors and parameters that can affect radiation dose and image quality and how they can be changed in the direction of dose reduction by designing or modifying scanning protocols.
CT parameters that affect the patient’s radiation dose are detector configuration, tube current, tube potential, pitch, patient positioning, scan range, reconstructed slice thickness, shielding (13).
CT Dose Optimization Strategies
In order CT examinations to comply with the “as far as reasonably practicable” principle, appropriate dose optimization strategies need to be developed.
CT machine manufacturers are striving to develop techniques to reduce radiation dose while providing diagnostic-quality images. New improved detectors, Automatic Exposure Control (AEC) systems and Iterative Reconstruction (IR) algorithms are the newest techniques for radiation dose optimization in CT diagnostics (14,15).
However, in a large proportion of CT studies submitted to the literature, CT examinations have been performed with multiphase scanning protocols that are not always appropriate according to the clinical indication. Additional phases effectively multiply the radiation dose, so multiphase trials are an important source of unnecessary additional radiation, especially if extrapolated to larger populations. The majority of patients were noted to have multiphase CT scans, with at least 1 phase which is not indicated (late phase or native non contrast series). Routine multiphase CT scans of the abdomen and pelvis can be considered a source of additional unnecessary radiation exposure because a large proportion of clinical indications concerning the abdominal viscera can be effectively addressed with a single portal-venous phase series, even in a clinical context of acute abdominal pain. This source of excess radiation can be corrected by a personalized approach to the patient’s needs and the correct choice of CT protocol according to the clinical question and the patient’s clinical condition and guided by the ACR Appropriateness Criteria or other evidence-based criteria (16,17). In doing so, the general guiding principles for optimization and dose reduction include Minimizing scan length; Use of tube current modulation; Minimizing tube current; Minimizing the potential; Tailoring a scan to a patient with appropriate scan phases; Scan series reduction; Iterative reconstruction; Periodic review of CT studies (18-20).
Conclusion
Optimization and CT dose reduction is a process of combining different approaches or strategies. These include adequate equipment selection and development of better exposure protocols by manufacturers, justifying the use of CT examination according to clinical indication and reducing unnecessary examinations, correct selection of the CT examination protocols and optimization of scanning protocols and adjustments according to age or weight, continuous training and education for the technologists, radiologists and medical physicists.
Achieving low-dose scanning is a team effort that requires tailoring the patient’s scan according to the medical question, continuously improving image quality while reducing the dose to the lowest possible level. Achieving this goal in practice requires a substantial knowledge base in the fields of radiation physics, biology and epidemiology, radiology and other various clinical applications.
References
1. Brenner DJ, Hall EJ. Computed tomography–an increasing source of radiation exposure. N Engl J Med. 2007 Nov 29;357(22):2277-84. doi: 10.1056/NEJMra072149. PMID: 18046031.
2. Westmark, S., Hessellund, T., Hoffmann, A et al. (2023). Increasing use of computed tomography scans in the North Denmark Region raises patient safety concern. European Journal of Radiology, 166, 110997.
https://doi.org/10.1016/j.ejrad.2023.110997
3. Pearce MS, Salotti JA, Little MP, et al. Radiation exposure from CT scans in childhood and subsequent risk of leukaemia and brain tumours: a retrospective cohort study. Lancet. 2012 Aug 4;380(9840):499-505. doi: 10.1016/S0140-6736(12)60815-0. Epub 2012 Jun 7. PMID: 22681860; PMCID: PMC3418594.
4. Hendel RC, Patel MR, Allen JM, et al. Appropriate use of cardiovascular technology: 2013 ACCF appropriate use criteria methodology update: a report of the American College of Cardiology Foundation appropriate use criteria task force. J Am Coll Cardiol. 2013 Mar 26;61(12):1305-17. doi: 10.1016/j.jacc.2013.01.025. Epub 2013 Feb 21. PMID: 23433633.
5. IAEA, International Atomic Energy Agency (2004) Optimisation of the radiological protection of patients undergoing radiography, fluoroscopy and computed tomography. Document no. IAEA-TECDOC-1423. Vienna, Austria: International Atomic Energy Agency.
6. Goo HW. CT radiation dose optimization and estimation: an update for radiologists. Korean J Radiol. 2012 Jan-Feb;13(1):1-11. doi: 10.3348/kjr.2012.13.1.1. Epub 2011 Dec 23. PMID: 22247630; PMCID: PMC3253393.
7. Smith-Bindman R, Lipson J, Marcus R,et al. Radiation dose associated with common computed tomography examinations and the associated lifetime attributable risk of cancer. Arch Intern Med. 2009 Dec 14;169(22):2078-86. doi: 10.1001/archinternmed.2009.427. PMID: 20008690.
8. Fazel R, Krumholz HM, Wang Y, Ross JS, et al. Exposure to low-dose ionizing radiation from medical imaging procedures. N Engl J Med. 2009 Aug 27;361(9):849-57. doi: 10.1056/NEJMoa0901249. PMID: 19710483; PMCID: PMC3707303.
9. Sodickson A, Baeyens PF, Andriole KP et al. Recurrent CT, cumulative radiation exposure, and associated radiation-induced cancer risks from CT of adults. Radiology. 2009 Apr;251(1):175-84. doi: 10.1148/radiol.2511081296. PMID: 19332852.
10. Wallace AB, Goergen SK, Schick D, Soblusky T, Jolley D. Multidetector CT dose: clinical practice improvement strategies from a successful optimization program. J Am Coll Radiol. 2010 Aug;7(8):614-24. doi: 10.1016/j.jacr.2010.03.015. Erratum in: J Am Coll Radiol. 2011 Apr;8(4):291. PMID: 20678731.
11. Boland GW, Duszak R Jr, Kalra M. Protocol design and optimization. J Am Coll Radiol. 2014 May;11(5):440-1. doi: 10.1016/j.jacr.2014.01.021. PMID: 24793037.
12. Tsapaki V, Aldrich JE, Sharma R, et al. Dose reduction in CT while maintaining diagnostic confidence: diagnostic reference levels at routine head, chest, and abdominal CT–IAEA-coordinated research project. Radiology. 2006 Sep;240(3):828-34. doi: 10.1148/radiol.2403050993. Epub 2006 Jul 12. PMID: 16837668.
13. Kalra A, Chakraborty A, Fine B, Reicher J. Machine learning for automation of radiology protocols for quality and efficiency improvement. J Am Coll Radiol. 2020; 17:1149–1158. doi: 10.1016/j.jacr.2020.03.012.
14. Arapakis I, Efstathopoulos E, Tsitsia V, et al. Using “iDose4” iterative reconstruction algorithm in adults’ chest-abdomen-pelvis CT examinations: effect on image quality in relation to patient radiation exposure. Br J Radiol. 2014 Apr;87(1036):20130613. doi: 10.1259/bjr.20130613. PMID: 24646183; PMCID: PMC4067031.
15. Baskan O, Erol C, Ozbek H, Paksoy Y. Effect of radiation dose reduction on image quality in adult head CT with noise-suppressing reconstruction system with a 256 slice MDCT. J Appl Clin Med Phys. 2015 May 8;16(3):5360. doi: 10.1120/jacmp.v16i3.5360. PMID: 26103494; PMCID: PMC5690139Raman SP, Mahesh M, Blasko RV, Fishman EK. CT scan parameters and radiation dose: practical advice for radiologists. J Am Coll Radiol. 2013 Nov;10(11):840-6. doi: 10.1016/j.jacr.2013.05.032. PMID: 24183553.
16. Little BP, Duong PA, Knighton J, Baugnon K at al. A Comprehensive CT Dose Reduction Program Using the ACR Dose Index Registry. J Am Coll Radiol. 2015 Dec;12(12 Pt A):1257-65. doi: 10.1016/j.jacr.2015.07.020. Epub 2015 Oct 21. PMID: 26475376.
17. Goenka AH, Dong F, Wildman B, Hulme K, Johnson P, Herts BR. CT Radiation Dose Optimization and Tracking Program at a Large Quaternary-Care Health Care System. J Am Coll Radiol. 2015 Jul;12(7):703-10. doi: 10.1016/j.jacr.2015.03.037. Epub 2015 May 21. PMID: 26003589.
18. Wallace AB, Goergen SK, Schick D, Soblusky T, Jolley D. Multidetector CT dose: clinical practice improvement strategies from a successful optimization program. J Am Coll Radiol. 2010 Aug;7(8):614-24. doi: 10.1016/j.jacr.2010.03.015. Erratum in: J Am Coll Radiol. 2011 Apr;8(4):291. PMID: 20678731.
19. Lira D, Padole A, Kalra MK, Singh S. Tube potential and CT radiation dose optimization. AJR Am J Roentgenol. 2015 Jan;204(1):W4-10. doi: 10.2214/AJR.14.13281. PMID: 25539272.
20. Guite KM, Hinshaw JL, Ranallo FN, Lindstrom MJ, Lee FT Jr. Ionizing radiation in abdominal CT: unindicated multiphase scans are an important source of medically unnecessary exposure. J Am Coll Radiol. 2011 Nov;8(11):756-61. doi: 10.1016/j.jacr.2011.05.011. PMID: 22051457; PMCID: PMC4131253.