UDK: 616.379-008.64-07(497.7)
Pre-consultation Stratification for Opportunistic Screening of Type 2 Diabetes in Primary Health Care: a Novel Approach in North Macedonia
Darko Iliev1, Petranka Mishevska1, Marija Vrca Botica2, Katarina Stavric1, Natasha Ilieva1, Irena Aleksioska Papestiev1.
Medical Faculty at “Ss. Cyril and Methodius” University, Skopje
Medical School Zagreb, Family Medicine, Croatia
Darko Iliev, MMSc, Family Medicine Specialist, Medical Faculty at “Ss. Cyril and Methodius” University, Skopje
Petranka Mishevska, PhD, Full Professor, University Clinic of Internal Medicine – Department for Gastroenterohepatology, Medical Faculty at “Ss. Cyril and Methodius” University, Skopje
Marija Vrca Botica, PhD, Full Professor, Department of Family Medicine, University of Zagreb, School of Medicine, Zagreb, Croatia
Katarina Stavric, PhD, Full Professor, Center for Family Medicine, Medical Faculty at Ss. Cyril and Methodius University, Skopje
Natasha Ilieva, MMSc, Teaching Assistant, University Clinic of Obstetrics and Gynecology, Medical Faculty at “Ss. Cyril and Methodius” University, Skopje
Irena Aleksioska Papestiev, PhD, Assistant Professor, University Clinic of Obstetrics and Gynecology, Medical Faculty at “Ss. Cyril and Methodius” University, Skopje
Corresponding author: Darko Iliev,
e-mail address: darko.iliev@gmail.com
Abstract
Introduction: Opportunistic screening for type 2 diabetes (T2D) is currently not a routine practice among family physicians in primary health care (PHC) settings. The efficiency and effectiveness of opportunistic screening approaches for T2D are critical due to the specific nature of PHC work. Stratifying patients with an increased risk of developing T2D in the pre-consultation phase can significantly streamline the process, enabling the identification and focus on high-risk groups.
Objective: This study aims to present the outcomes of patients’ stratification in the pre-consultation phase of opportunistic screening for type 2 diabetes.
Materials and Methods: Utilizing an electronic program, each participating physician selected patients aged 45-70 years. During December 2016 – January 2017, a pre-consultation phase questionnaire was completed for each patient, categorizing them into four groups: patients at risk of developing T2D, patients without risk for T2D, patients without sufficient data, and excluded patients based on exclusion criteria.
Results: The study involved 25 doctors from various cities across the Republic of Macedonia, covering a total of 41,836 registered patients. The analysis focused on 14,154 patients within the 45 – 70 years age group. Out of these, 8,754 patients were excluded based on exclusion criteria, 1,354 patients did not have any risk factors for T2D, 1,329 patients were excluded due to incomplete data on risk factors, and 2,659 patients had multiple risk factors for T2D and were included in the screening group.
Conclusion: The pre-consultation phase stratification effectively identified a subset of patients at higher risk for type 2 diabetes, facilitating targeted opportunistic screening. This approach could enhance the efficiency of T2D screening in PHC settings and potentially improve early detection and management of the disease in North Macedonia.
Key Words: Diabetes Mellitus Type 2, Early Diagnosis, Electronic Medical Records, Family Practice, North Macedonia, Opportunistic Screening, Patient Stratification, Pre-consultation, Primary Health Care, Risk Assessment.
Introduction
The global incidence of type 2 diabetes (T2D) is constantly increasing at the global level (Ogursova et al., 2022). In our country, the rate of people with type 2 diabetes is 7.2% in 2019 (Ahmeti et al., 2020). The condition of long-term elevated glycemia in patients causes a long-term severe and progressive disease, causing severe complications with the possibility of developing disability and is the fifth cause of death in developed countries and ninth leading cause of mortality globally (Spijkerman et al., 2003; Standl et al., 2019; Abdul Basith Khan et al., 2020). Before T2D develops, there is a so-called prediabetes condition, which implies a disturbance of fasting glycemia with values between 5.6-6.9 mmol/L and 7.8-11.1 mmol/L measured after a 75-g oral glucose load, according to the American Diabetes Association (Echouffo-Tcheugui et al., 2023; Buysschaert et al., 2016). According to World Health Organization, also International Diabetes Association recommends fasting plasma glucose levels of 6.1-6.9mmol/l (van Herpt et al., 2020; Sulaiman & Labib, 2010). Up to 10% of these patients will develop diabetes within 1 year. If T2D is diagnosed and treated promptly, there is a percentage of patients in whom the risk of complications will be reduced and they may even convert to normoglycemia as soon as the onset of the disease is delayed (Ligthart et al., 2015). In order to be able to treat T2D, it must be first recognized or diagnosed (Drobek et al., 2021).
In our country, population screening is currently being carried out as a preventive goal among general practitioners for early detection of diabetes (FZOM, 2024). It is performed for the entire population aged 35-56 without exception. A scored questionnaire of the Finnish Prevention Study (FINDRISC) is used, which consists of the following questions: age, body mass index, waist circumference, physical activity, consumption of fruits and vegetables, use of antihypertensive therapy, history of measured elevated glycemia, family burden with diabetes. Depending on the scores, the patients are categorized into 5 categories: low, slightly elevated, moderately elevated, high and very high risk, where slightly elevated and moderately elevated risk are sent for an oral glucose tolerance test, and high and very high are referred to a higher level of health care (Gabriel et al., 2021).
This type of screening involves high costs, workload for family doctors, and is not in accordance with the latest recommendations (ADA, 2020; ElSayed et al., 2023). The experience so far shows that fasting glucose determination as a campaign for the entire population does not achieve the desired coverage and the effect is “low cost-benefit”, which would mean that in the total examined population, the proportion of detected is small in proportion to the number of covered patients (Zhou et al., 2020; Khunti et al., 2012).
Clinically opportunistic screening for T2D is widely accepted as an approach and is defined as a process in which the physician uses the consultation for any patient that needs to investigate the possibility of T2D or prediabetes (Selph et al., 2015). For the general population, the general or family doctor is the first stop when any health problem appears. The efficiency and effectiveness of the approach to opportunistic screening for T2D in the work of Primary Health Care (PHC) doctors is crucial due to the specifics of their work, such as large number of patients, lack of time, financial efficiency, etc. By stratifying patients with an increased risk of developing T2D who would further be called to do a laboratory test of fasting glycemia, the number of those who will be tested is limited (Ashenhurst et al., 2022; Greaves et al., 2004). Although at this moment part of the information is entered electronically, there are no appropriate tools and mechanisms in our country, for directly selecting patients with certain risk factors and conditions that are required for this stratification, and some of the risk factors are not subject to electronic entry at all (Smokovski & Smokovski, 2021). Information from patients’ charts can be used to stratify patients, especially in low-and-middle income countries (Masyuko et al., 2021).
The objective of this study is to evaluate the feasibility and effectiveness of stratifying patients based on risk factors for type 2 diabetes (T2D) in the pre-consultation phase within primary healthcare settings in North Macedonia. By utilizing data from electronic health records and patients’ card files, the study aims to identify high-risk individuals aged 45-70 years and assess the impact of targeted screening on early detection rates of T2D. Additionally, the study seeks to highlight gaps in current data collection practices and propose improvements to enhance the accuracy and efficiency of risk stratification, ultimately contributing to better management and prevention of T2D in the primary care context.
Material and Method
This study utilized a cross-sectional design to evaluate the stratification of patients based on risk factors for type 2 diabetes (T2D) in primary healthcare settings across North Macedonia. The study was conducted in collaboration with 25 general practitioners from urban and rural areas, covering 17 municipalities (Bitola, Gazi Baba, Gevgelija, Gjorce Petrov, Gostivar, Kavadarci, Karposh, Kochani, Kumanovo, Makedonska Kamenica, Prilep, Radovish, Saraj, Strumica, Tetovo, Centar and Shtip). Majority of specialists in family medicine applied for a call published in cooperation with the Center for Family Medicine. All of them work as family doctors in agreement with the Health Insurance Fund (FZOM).
Participants and Data Collection:
The participating doctors were enrolled through an electronic call for participation. Data were collected from an electronic health program used for guiding patients’ management according to the requirements of the Health Insurance Fund (FZOM), as well as from patients’ card files. The information included demographic details, family history of diabetes, history of gestational diabetes, previous glycemia measurements, presence of hypertension, hyperlipidemia and body mass index (BMI). With the help of a questionnaire for the pre-consultation phase that was prepared according to the submission for the preparation of this study and aligned with the latest recommendations, each doctor filled out a questionnaire for all patients aged 45-70 years who were selected using the electronic program. The data is filled in from the patients’ files and the empirical knowledge of the patients by the doctor. Coding of the patients is done in the first part of the questionnaire by entering the patient’s card number and initials as a source for verification and validation of the questionnaire itself with confirmation by facsimile by the family physician. In the first part of the questionnaire, the following questions are included: card number and initials for verification of the patients with the doctor’s facsimile number, then gender and age and the following exclusion criteria: age under 45 years, have been diagnosed with T2D, pregnancy at the moment, if in the last 3 years all glycemic measurements were <6mmol/L and persons with impaired consciousness and judgment.
Risk Factor Stratification:
In the second part of the questionnaire, in accordance with the recommendations of the ADA and the IDF, the following risk factors for the occurrence of T2D were taken into account (ADA, 2020; IDF, 2017):
- Type 2 diabetes within a close family (parents, brothers and sisters),
- Hypertension,
- High body mass index BMI (>25),
- Hyperlipidemia,
- Gestational diabetes (in pregnant women) or a child born weighing more than 4000g,
- Glycemia measured in the last 3 years with a value between 6.1-7.0mmol/l.
Depending on the answers in the questionnaire, the patients were divided into 4 groups of patients:
- Group of patients who will not be screened due to exclusion criteria,
- Group of patients who, apart from age, have at least one other risk factor for the development of T2D and who will be screened (a person may have one or more risk factors);
- Group of patients who, apart from age, have no additional risk factors for the development of T2D and in whom screening will not be done,
- Group of patients who will not be screened due to lack of data.
Regarding the way of working in this study, a meeting was held at the beginning of December 2016 where the study was presented and possible challenges in its work were discussed. A manual has also been prepared and the same was given in addition to each doctor.
All completed questionnaires were returned to the Center for Family Medicine at the end of January 2017 and in the period February – March 2017 they were entered into a database created according to the questionnaire. Only patients who, apart from age, have another risk factors for the development of T2D and in whom screening would be done, the questionnaires remained with the doctors for the second phase/ consultation.
The data were entered in an excel table and coded with numbers according to the coding of the questionnaire.
Statistical Methods:
Descriptive statistics were used to summarize the demographic characteristics and risk factor prevalence in both groups. Chi-square tests and t-tests were employed to compare the differences between screened and non-screened groups. Statistical significance was set at p<0.05. All analyses were performed using SPSS software, version 25.0.
This methodological approach aimed to provide comprehensive insights into the current state of risk stratification for T2D in primary healthcare and propose recommendations for enhancing early detection and management practices.
Results
Twenty-five doctors from urban and rural areas, representing 17 municipalities (Bitola, Gazi Baba, Gevgelija, Gjorce Petrov, Gostivar, Kavadarci, Karposh, Kochani, Kumanovo, Makedonska Kamenica, Prilep, Radovish, Saraj, Strumica, Tetovo, Centar and Shtip), participated in this study. These physicians were enrolled through an electronic call for participation. Data were collected using an electronic program designed to guide patients according to the requirements of the Health Insurance Fund (FZOM) and from patients’ records. The information utilized included data present in the electronic program, as well as the doctors’ personal knowledge and assessments of their patients.
The average number of patients managed by these doctors is 1,673. Within the risk group aged 45-70 years, there were a total of 14,154 patients, averaging 565 (33%) patients per doctor. The screening group comprises 2,659 patients, representing 18.79% of the entire population aged 45-70 years. This group includes patients with at least one positive risk factor out of six identified risk factors, and they would be offered screening during their next visit to the doctor. Given the uncertainty of the timing of the next visit and the potential for additional risk factors to be documented for some patients, these questionnaires will remain with the doctors and are not included in the analysis presented in this report.
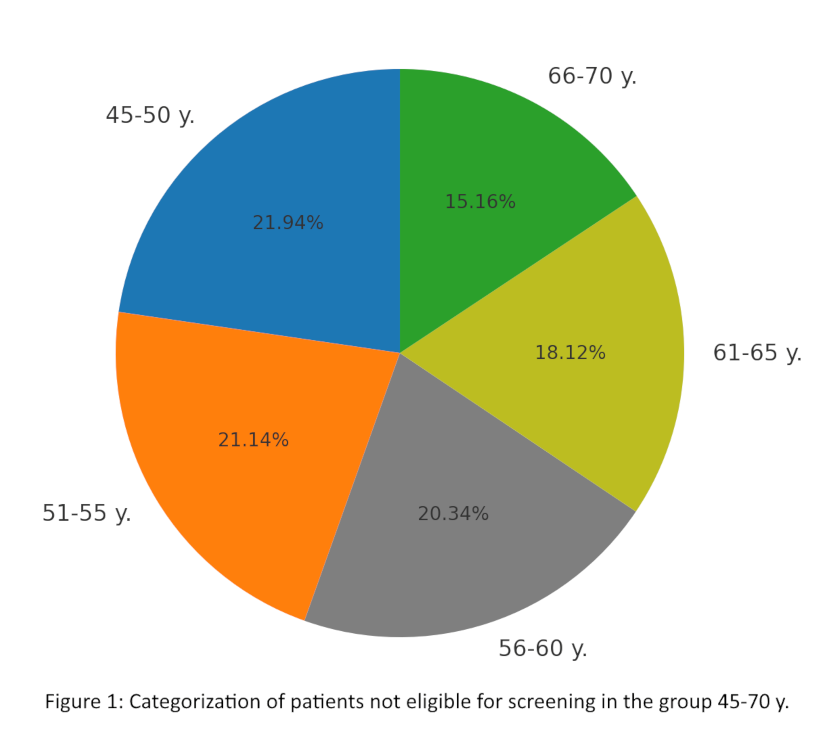
The analysis includes 11,495 patients (81.21% of the category aged 45-70 years) who were excluded from the screening group. This cohort exhibits a nearly equal gender distribution, with 5,482 (47.89%) men and 5,726 (50.02%) women. Chart 1 illustrates the age distribution of the excluded patients, which shows a consistent distribution across age decades: 2,453 (21.94%) in the 45-50 years group, 2,364 (21.14%) in the 51-55 years group, 2,274 (20.34%) in the 56-60 years group, 2,026 (18.12%) in the 61-65 years group, and 1,695 (15.16%) in the 66-70 years group.
Chart 1. Categorization of patients not eligible for screening in the group 45-70 years old.
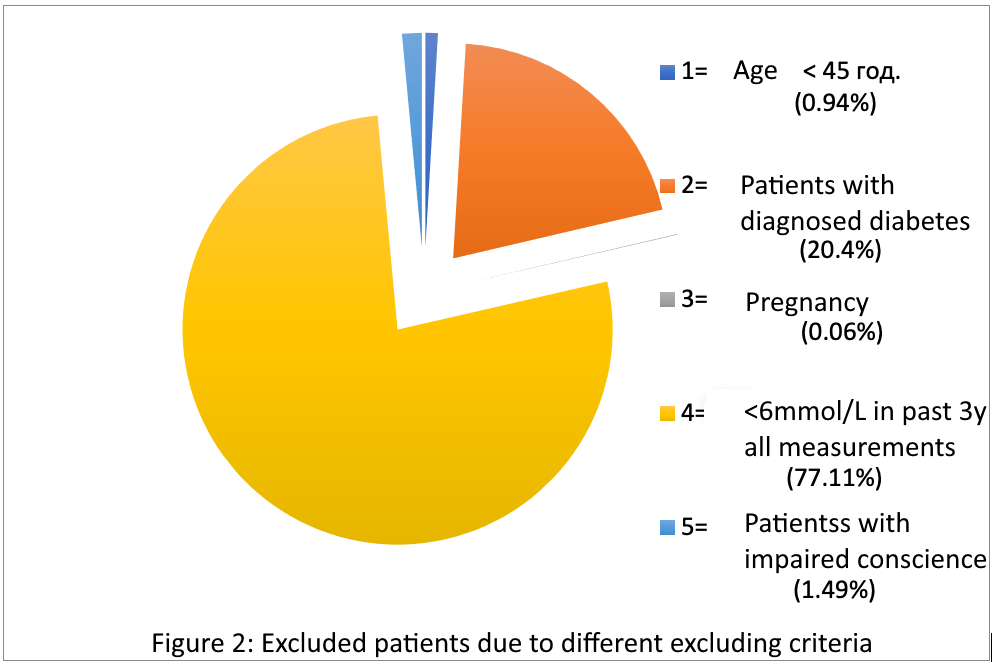
Stratification of the patients excluded from screening, due to exclusion criteria, identified that 8,754 patients (61.9%) belong to the 45-70 years age group. Chart 2 shows these patients divided to subsequent categories.
Chart 2. Excluded patients due to different excluding criteria.
Of these, 2,693 (19%) patients either lack a risk factor or have incomplete risk factor data. Within this subset, 1,364 (50.65%) have complete data indicating no presence of risk factors, 931 (34.57%) lack information on one or more risk factors, but have no identified risk factors, and 398 (14.78%) have no data regarding the presence or absence of any risk factors.
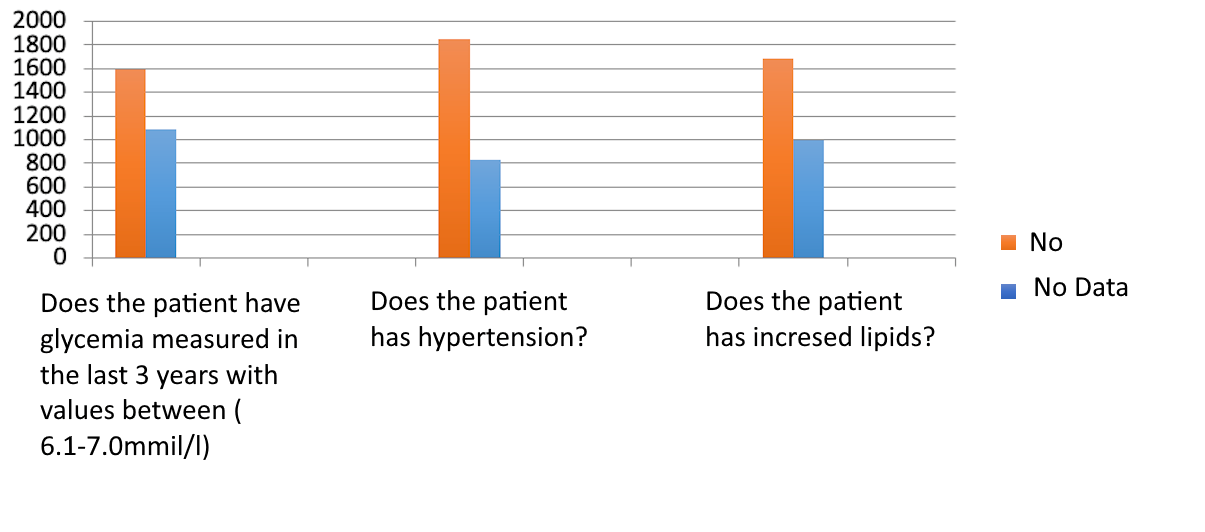
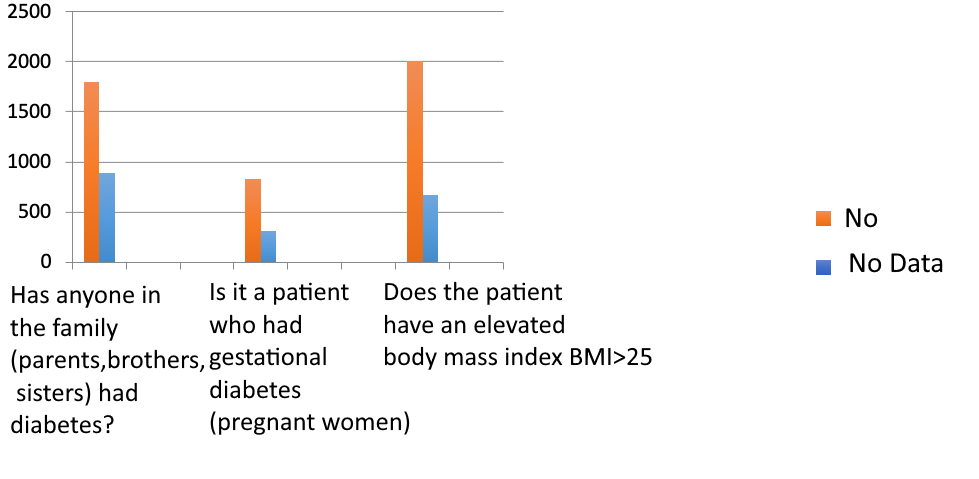
Chart 3 displays the distribution of responses regarding the presence of risk factors among the group that will not undergo screening, highlighting the ratios of ‘NO’ and ‘NO DATA’ responses. Among the six risk factors assessed, 1,329 (49.35%) patients did not respond to one or more questions out of the total 2,693 patients. Consequently, these patients are excluded from the screening group due to either the absence of risk factors or incomplete data on one or more risk factors.
Chart 3. Distribution of responses regarding the presence of risk factors among the group that will not undergo screening, highlighting the ratios of ‘NO” and ‘NO DATA’.
The findings from this study underscore the significance of risk stratification in the pre-consultation phase for opportunistic screening of type 2 diabetes. The identification of 2,659 patients with at least one risk factor emphasizes the need for targeted screening approaches in primary healthcare settings. This group, which represents 18.79% of the population aged 45-70 years, illustrates the potential for early intervention and management of type 2 diabetes, thereby reducing long-term healthcare costs and improving patients’ outcomes.
Conversely, the substantial number of patients (11,495 or 81.21%) excluded from the screening group provides insight into the current health status and risk factor prevalence in the broader patient population. The nearly equal gender distribution and consistent age distribution across age groups indicate a uniform representation of the population in this study (Table 1).
Table 1. Summarized data of the study findings.
| Category | Number of Patients | Percentage of Total (%) |
| Total Patients Managed by Doctors | – | – |
| Average Number of Patients per Doctor | 1,673 | – |
| Patients Aged 45-70 Years | 14,154 | 100 |
| Screening Group | 2,659 | 18.79 |
| Excluded from Screening | 11,495 | 81.21 |
| Excluded Patients’ Gender Distribution | ||
| – Men | 5,482 | 47.89 |
| – Women | 5,726 | 50.02 |
| Excluded Patients’ Age Distribution | ||
| – Ages 45-50 | 2,453 | 21.94 |
| – Ages 51-55 | 2,364 | 21.14 |
| – Ages 56-60 | 2,274 | 20.34 |
| – Ages 61-65 | 2,026 | 18.12 |
| – Ages 66-70 | 1,695 | 15.16 |
| Risk Factors Data among Excluded Patients | ||
| – No Risk Factors | 1,364 | 50.65 |
| – Incomplete Data on Risk Factors | 931 | 34.57 |
| – No Data on Risk Factors | 398 | 14.78 |
The detailed stratification of excluded patients reveals critical gaps in data collection and risk factor documentation. The fact that 2,693 patients (19%) either lack risk factors or have incomplete risk factor data highlights the necessity for comprehensive patients’ records and systematic data entry practices. Moreover, the identification of subgroups within this cohort—those with no risk factors, incomplete data on one or more risk factors, and those with entirely missing data on all risk factors—points to areas where healthcare practices can be improved to ensure accurate risk assessment and appropriate screening.
Discussion
This approach of stratifying patients for the presence of a risk factor for the development of T2D is easily feasible in the daily practice of a general family medicine physician. Paradox is the situation in which early diagnosis and prevention of diseases is supported in principle, but not implemented in practice (Bergman, 2016). The situation is more concerning in low-and-middle income countries, which lack data regarding this common disease and its screening (Correia et al., 2019; Manne-Goehier et al., 2019). Part of the reason for this is that neither the electronic database nor the card file systematically records all the data that represents a risk factor. Due to this situation, there is a possibility that some patients are left out of the screening and belong to a risk group, but there is simply not enough data about them. This is shown by the data from the group of patients who would not be screened because they either have no risk factors or no data. Oot of these, 33.12% of patients did not have data on the presence of diabetes in the family history (in the literature, about 15%)(Sterne et al., 2009; Aizpuru et al., 2012), in 27.24% of women therewas no data on whether it is a patient who had had gestational diabetes or a child born with a weight greater than 4000g, 40% did not have data on measured glycemia in the past 3 years, about 30.7% of the patients did not have data on the presence of hypertension, 33% on hyperlipidemia, and 27% did not have data on body mass index. This condition was also present in the CroDiab study (Vrca Botica et al., 2017), which applied a similar approach. Apart from the absence of structured data entry as the reason for the lack of data on all risk factors, the situation when patients did not visit their doctor for a long time for various reasons (moving, travel, work duties, inadequate care for their health, distance of the doctor, etc.), as well as the workload of the doctors (Xiong et al., 2023).
In the second stage (screening) the patients with risk factors enter 2,659 (18.7%) patients who would give answers regarding the incidence of T2D and distribution by region, age and sex, as well as the connection with the mentioned risk factors. The analysis of risk factors in this group will be done after the completion of the study.
Due to previously diagnosed T2D, 12.6% of patients aged 45-70 years were excluded from the study, which indicates a higher prevalence of diabetes in this age group compared to the national one (IDF, 2019). Furthermore, almost half of the total number of patients aged 45-70 years, 47.69% (in the literature 20.5%), are excluded due to the fact that all glycemia measurements in the past years are below 6mmol/l (normoglycemia). This is due to the preventive goals that doctors work in agreement with FZOM for early detection of type 2 diabetes by means of population screening, which is an example of the positive effects of early diagnosis in general (Koller et al., 2024; Aizpuru et al., 2012).
The advantage of this approach is the stratification by risk factors itself, where 81.3% (77.5% in CroDiabGP) of patients do not enter the screening group even in the pre-consultation phase, which is expected to give greater sensitivity to further screening and greater cost efficiency in the same access (Botica et al., 2017). If it is possible to enter structured data into the electronic database of doctors, it will be possible to select patients according to risk factors and it would be much simpler to get the most suitable candidates for screening in the pre-consultation phase for further glycemic testing.
These findings suggest that enhancing electronic health record systems and implementing standardized data entry protocols could significantly improve the accuracy and efficiency of risk stratification in primary healthcare. Future research should focus on developing and testing interventions aimed at addressing these data gaps and evaluating their impact on screening and patients’ outcomes in type 2 diabetes management (Carpenter et al., 2019).
Conclusion
This study highlights the feasibility and importance of stratifying patients based on risk factors for type 2 diabetes (T2D) in primary healthcare settings. The findings demonstrate that a significant proportion of patients (81.21%) were excluded from screening due to the absence of risk factors or incomplete data, underscoring the need for comprehensive and systematic data entry. The exclusion of nearly half the patients due to normoglycemia reflects the effectiveness of ongoing preventive measures. Enhancing electronic health record systems and standardizing data entry protocols are essential to improve risk stratification accuracy and screening efficiency. Future efforts should focus on closing data gaps and evaluating interventions to optimize patient outcomes in T2D management. This approach can lead to early diagnosis, timely intervention, and better healthcare resource utilization, ultimately reducing the burden of T2D.
References
- Abdul Basith Khan, M., Hashim, M.J., King, J.K., Govender, R.D., Mustafa, H. and Al Kaabi, J., 2020. Epidemiology of type 2 diabetes—global burden of disease and forecasted trends. Journal of epidemiology and global health, 10(1), pp.107-111.
- Ahmeti, I., Bitovska, I., Markovic, S., Sukarova-Angelovska, E., Jovanovska-Misevska, S. and Kocinski, G., 2020. Growing prevalence and incidence of diabetes in republic of macedonia in the past 5 years based on data from the national system for electronic health records. Open Access Macedonian Journal of Medical Sciences, 8(B), pp.643-645.
- Aizpuru, F., Latorre, A., Ibáñez, B., Garcia, K.L., Vergara, I., Pz de Arriba, J., Samper, R., López-Picado, A., Apiñaniz, A. and Bilbao, J.L., 2012. Variability in the detection and monitoring of chronic patients in primary care according to what is registered in the electronic health record. Family practice, 29(6), pp.696-705.
- American Diabetes Association, 2020. 2. Classification and diagnosis of diabetes: standards of medical care in diabetes—2020. Diabetes care, 43(Supplement_1), pp.S14-S31.
- Ashenhurst, J.R., Sazonova, O.V., Svrchek, O., Detweiler, S., Kita, R., Babalola, L., McIntyre, M., Aslibekyan, S., Fontanillas, P., Shringarpure, S. and 23andMe Research Team, 2022. A polygenic score for type 2 diabetes improves risk stratification beyond current clinical screening factors in an ancestrally diverse sample. Frontiers in Genetics, 13, p.871260.
- Bergman M. Controversies and current approaches in the diagnosis of prediabetes and diabetes mellitus. Curr Diabetes Rev 2016;12(1):1e6.
- Botica, M.V., Carcaxhiu, L., Kern, J., Kuehlein, T., Botica, I., Gavran, L., Zelić, I., Iliev, D., Haralović, D. and Vrca10, A., 2017. Missing risks in opportunistic screening for type 2 diabetes-CroDiabGP study. Med Glas (Zenica), 14(1), pp.55-60.
- Buysschaert, M., Medina, J.L., Buysschaert, B. and Bergman, M., 2016. Definitions (and current controversies) of diabetes and prediabetes. Current diabetes reviews, 12(1), pp.8-13.
- Carpenter, R., DiChiacchio, T. and Barker, K., 2019. Interventions for self-management of type 2 diabetes: An integrative review. International journal of nursing sciences, 6(1), pp.70-91.
- Correia, J.C., Lachat, S., Lagger, G., Chappuis, F., Golay, A., Beran, D. and COHESION Project David Beran Jaime Miranda Albertino Damasceno Claire Somerville L. Suzanne Suggs, 2019. Interventions targeting hypertension and diabetes mellitus at community and primary healthcare level in low-and middle-income countries: a scoping review. BMC Public Health, 19, pp.1-20.
- Drobek, N., Sowa, P., Jankowski, P., Haberka, M., Gąsior, Z., Kosior, D., Czarnecka, D., Pająk, A., Szostak-Janiak, K., Krzykwa, A. and Setny, M., 2021. Undiagnosed diabetes and prediabetes in patients with chronic coronary syndromes—An alarming public health issue. Journal of Clinical Medicine, 10(9), p.1981.
- Echouffo-Tcheugui, J.B., Perreault, L., Ji, L. and Dagogo-Jack, S., 2023. Diagnosis and management of prediabetes: a review. Jama, 329(14), pp.1206-1216.
- ElSayed, N.A., Aleppo, G., Aroda, V.R., Bannuru, R.R., Brown, F.M., Bruemmer, D., Collins, B.S., Gaglia, J.L., Hilliard, M.E., Isaacs, D. and Johnson, E.L., 2023. 2. Classification and diagnosis of diabetes: standards of care in diabetes—2023. Diabetes care, 46(Supplement_1), pp.S19-S40.
- FZOM, MK, Template for prevention and early detection of diabetes melitus. Accessed on: 01.03.2024; Available at: http://www.fzo.org.mk/WBStorage/Files/Obrazec_za_prevencija_na_dijabetes_od_35_do_56_god..pdf.
- Gabriel, R., Acosta, T., Florez, K., Anillo, L., Navarro, E., Boukichou, N., Acosta-Reyes, J., Barengo, N.C., Lindström, J., Tuomilehto, J.O. and Aschner, P., 2021. Validation of the Finnish type 2 diabetes risk score (FINDRISC) with the OGTT in health care practices in Europe. Diabetes Research and Clinical Practice, 178, p.108976.
- Greaves, C. et al. A simple pragmatic system for detecting new cases of type 2 diabetes and impaired fasting glycaemia in primary care. Fam. Pract.21, 57–62 (2004).
- International Diabetes Federation. Recommendations For Manag- ing Type 2 Diabetes In Primary Care, 2017. Available at: idf.org/managing-type2-diabetes; Accessed on: 13.04.2024.
- International Diabetes Federation (IDF). IDF Diabetes Atlas 9th edition. org (2019). doi:10.1289/image.ehp.v119.i03. Available at: https://diabetesatlas.org/idfawp/resource-files/2019/07/IDF_diabetes_atlas_ninth_edition_en.pdf; Accessed on: 02.02.2024.
- Khunti K, Gilles CL, Taub NA, Mostafa SA, Hiles SL,Abrams KR, et al. A comparision of cost per case detected of screening strategies for type 2 diabetes and impaired glucose regulation: modeling study. Diabetes Res Clin Pract 2012;97:505e13.
- Koller, T.S., Janeva, J.K., Ognenovska, E., Vasilevska, A., Atanasova, S., Brown, C., Dedeu, A. and Johansen, A., 2024. Towards leaving no one behind in North Macedonia: a mixed methods assessment of barriers to effective coverage with health services. International Journal for Equity in Health, 23(1), p.58.
- Ligthart S, Herpt TTW, Leening MJG, Kavousi M, Hofman A, Stricker BHC, et al. Lifetime risk of developing impaired glucose metabolism and eventual progression from prediabetes to type 2 diabetes: a prospective cohort study. Lancet Diabetes @ Endocrinoloc 2015;4(1):44e51. http:// dx.doi.org/10.1016/S2213-8587(15)00362-9.
- Masyuko, S., Ngongo, C.J., Smith, C. and Nugent, R., 2021. Patient-reported outcomes for diabetes and hypertension care in low-and middle-income countries: a scoping review. PLoS One, 16(1), p.e0245269.
- Ogurtsova, K., Guariguata, L., Barengo, N.C., Ruiz, P.L.D., Sacre, J.W., Karuranga, S., Sun, H., Boyko, E.J. and Magliano, D.J., 2022. IDF diabetes Atlas: Global estimates of undiagnosed diabetes in adults for 2021. Diabetes research and clinical practice, 183, p.109118.
- Selph, S. et al. Screening for type 2 diabetes mellitus: a systematic review for the U.S. Preventive Services Task Force. Ann. Intern. Med.162, 765–76 (2015).
- Smokovski, I. and Smokovski, I., 2021. Benefits of Centralized e-Health System in Diabetes Care. Managing Diabetes in Low Income Countries: Providing Sustainable Diabetes Care with Limited Resources, pp.73-83.
- Spijkerman, A. M. W. et al. Microvascular complications at time of diagnosis of type 2 diabetes are similar among diabetic patients detected by targeted screening and patients newly diagnosed in general practice: the hoorn screening study. Diabetes Care26, 2604–8 (2003).
- Sterne JAC, White IR, Carlin JB, Spratt M, Royston P, Kenward MG, et al. Multiple imputation for missing data in epidemiological and clinical research: potential and pitfalls. BMJ 2009;338. http://dx.doi.org/10.1136/bmj.b2393.
- van Herpt, T.T., Ligthart, S., Leening, M.J., van Hoek, M., Lieverse, A.G., Ikram, M.A., Sijbrands, E.J., Dehghan, A. and Kavousi, M., 2020. Lifetime risk to progress from pre-diabetes to type 2 diabetes among women and men: comparison between American Diabetes Association and World Health Organization diagnostic criteria. BMJ Open Diabetes Research and Care, 8(2), p.e001529.
- Vrca Botica M, Carcaxhiu L, Kern J, Kuehlein T, Botica I, Gavran L, et al. Missing risks in opportunistic screening for type 2 diabetesdCroDiabGP study. Med Glas (Zenica) 2017;14(1). http://dx.doi.org/10.17392/874-16.
- World Health Organization, 1999. Definition, diagnosis and classification of diabetes mellitus and its complications: report of a WHO consultation. Part 1, Diagnosis and classification of diabetes mellitus (No. WHO/NCD/NCS/99.2). World health organization. Accessed on: 01.03.2024; Available at: https://iris.who.int/bitstream/handle/10665/66040/?sequence=1.
- Xiong, S., Jiang, W., Meng, R., Hu, C., Liao, H., Wang, Y., Cai, C., Zhang, X., Ye, P., Ma, Y. and Liu, T., 2023. Factors associated with the uptake of national essential public health service package for hypertension and type-2 diabetes management in China’s primary health care system: a mixed-methods study. The Lancet Regional Health–Western Pacific, 31.
- Zhou, X., Siegel, K.R., Ng, B.P., Jawanda, S., Proia, K.K., Zhang, X., Albright, A.L. and Zhang, P., 2020. Cost-effectiveness of diabetes prevention interventions targeting high-risk individuals and whole populations: a systematic review. Diabetes Care, 43(7), pp.1593-1616.