UDK: 616.24-031.4-085.816.2:616.24-006.6-089.87-06
https://www.doi.org/10.55302/MJA2484035k
Kokareva A1, Brzanov-Gavrilovska A1, Kondov G2, Jovanova S3, Buntashevska B1, Jovanovski-Srceva M1
1University Clinic for Traumatology, Orthopedic Diseases, Anesthesiology, Reanimation and Intensive Care Medicine and Emergency Department, Clinical Center “MotherTheresa” Faculty of Medicine, “Ss. Cyril and Methodius” University, Skopje, Republic of North Macedonia
2University Clinic for Thoracic and Vascular Surgery, “Ss. Cyril and Methodius” University, Skopje
3University Clinic for Cardiology, “Ss. Cyril and Methodius” University, Skopje
Abstract
Introduction: On one hand, one-lung ventilation is a method intended to improve surgical access while guaranteeing enough oxygenation and is often required for thoracic surgery. On the other hand, one-lung ventilation increases the risk of pulmonary complications both during and after surgery. Because they raise morbidity, lengthen hospital stays and may have negative consequences, these complications are clinically significant. Our evaluation’s goal was to determine the frequency and predictors of these complications, which are crucial for enhancing patient care and maximizing surgical results.
Material and Methods:In this retrospective analysis, we assessed 80 elective patients who had one-lung ventilation and lung resection as a result of cancer. The anesthetic protocol for all patients followed a standardized approach, ensuring consistency in perioperative management. The defined inclusion and exclusion criteria were used to determine which patients were included in the study. We looked at pulmonary complications after surgery, such as respiratory insufficiency, pneumonia and atelectasis in the first week after surgery.
Results: The study included 80 patients, with a postoperative pulmonary complication rate of 30.0%. Atelectasis, pneumonia and respiratory failure were the most commonly observed complications, with pneumonia being the leading cause. Pulmonary complications were significantly more prevalent in patients undergoing lobectomy (79.2%) and in those over 60 years of age (75.0%). Male gender, higher BMI (>25), reduced FEV1% (<70) and FVC (<70) significantly increased the risk of pulmonary complications. Although oxygen saturation (SpO2%) dropped during one-lung ventilation, this was more pronounced on the right side, though without statistical significance.
Conclusion: It is very common for pulmonary complications to happen after thoracic surgery. This is mostly because of the physiological changes that happen in the operating room and the use of one-lung ventilation. These factors significantly impact respiratory mechanics and gas exchange, underscoring the need for vigilant perioperative monitoring and tailored management strategies to mitigate these complications.
Keywords: atelectasis; one-lung ventilation; pneumonia; pulmonary complications; respiratory failure.
Introduction
Anesthesia in thoracic surgery is inconceivable without the use of one-lung ventilation (OLV), which facilitates optimal surgical exposure. Typically achieved through the insertion of a double-lumen endotracheal tube or a bronchial blocker, OLV allows ventilation of a single lung while maintaining perfusion in both. But this method makes big changes to the lungs’ physiology, like a ventilation/perfusion (V/Q) mismatch and intrapulmonary shunting, which can compromise oxygenation and raise the risk of pulmonary complications like atelectasis, pneumonia, and respiratory failure after surgery (1).
Multiple factors, including proper tube placement, the use of a bronchoscope, the patient’s underlying respiratory status, body positioning during surgery, the type of surgical procedure, ventilator settings and the anesthesiologist’s expertise in thoracic surgery, influence the risk of pulmonary complications during OLV (2,3). Hypoxemia, which is a drop in arterial oxygen saturation (SpO₂) below 90% as measured by pulse oximetry, may also happen during OLV, making patients even more likely to have pulmonary complications and bad outcomes after surgery (4).
Patients undergoing thoracic surgery often have pre-existing pulmonary and systemic comorbidities, such as chronic obstructive pulmonary disease (COPD), coronary artery disease, or anemia. These conditions, combined with the physiological challenges of OLV, can increase the likelihood of complications, including prolonged mechanical ventilation, pneumonia, atelectasis and acute respiratory distress syndrome (ARDS). Such complications can significantly compromise recovery and increase morbidity and mortality rates (5).
Preoperative risk assessment is crucial for identifying patients at high risk of developing postoperative pulmonary complications. Functional evaluations, including spirometry and arterial blood gas analysis, remain essential tools to assess pulmonary reserve and gas exchange capacity. Nonetheless, preoperative testing is a cornerstone of thoracic surgical planning to optimize patients’ outcomes (6-9). Our evaluation’s goal was to determine the frequency and predictors of these pulmonary complications, which are crucial for enhancing patient care and maximizing surgical results.
Material and Methods
The Clinic for Thoracic and Vascular Surgery in Skopje conducted this retrospective/ prospective observational study over the course of a year (2022–2023). Eighty patients underwent standard lung resection procedures (segmentectomy, lobectomy, bilobectomy and pneumonectomy) to treat lung cancer. These procedures were done with a double-lumen endotracheal tube (DLT) and general anesthesia.
Patients who met the ASA I–III classification, had an ejection fraction (EF) of at least 50%, hemoglobin levels of at least 90g/L, and had not been through any chemotherapy or radiation cycles before were eligible to take part. Patients with endocrinopathies, pathological arrhythmias, metastatic abnormalities in the contralateral lung, or significant pre-existing pulmonary impairment, such as a FEV₁ of less than 40% before surgery, were not eligible. The clinical ethics council granted ethical permission for the trial, and each participant gave their informed consent.
Every patient had the same anesthetic regimen. The thorough preoperative examinations included the patient’s history, a clinical examination that focused on the respiratory and cardiovascular systems, a measurement of body weight and height, a measurement of non-invasive blood pressure (NIBP), and a computation of the optimal body mass index (BMI). A 12-lead electrocardiogram (ECG), preoperative echocardiogram, routine laboratory testing, imaging examinations such as chest computed tomography (CT), and a baseline pulmonary function assessment were among the other assessments. We performed standard preoperative procedures, including premedication with 5mg diazepam tablets and fasting.
We monitored all patients intraoperatively with standard parameters such as an arterial line, NIBP, pulse oximetry and ECG. We used an epidural catheter to provide postoperative analgesia. We used a consistent protocol to induce general anesthesia, administering 2mg midazolam, 3g/kg fentanyl, and 1-2mg/kg propofol. We then administered rocuronium bromide (0.6mg/kg) to relax the muscles and facilitate the placement of the DLT. We used auscultation and bronchoscopy to verify the correct positioning of the DLT.
We used a continuous infusion of propofol (6–7mg/kg/h), intermittent fentanyl (2g/kg), and rocuronium (0.3mg/kg/h) to maintain anesthesia during the procedure. Tidal volumes of 7ml/kg of ideal body weight during two-lung ventilation (TLV) were lowered to 5ml/kg during one-lung ventilation (OLV), with PEEP set to 5cmH2O and a FiO₂ of 0.5. We modified these ventilation parameters based on the stage of operation. We adjusted other ventilatory parameters, such as respiratory rates and inspiratory-to-expiratory ratios, as needed to maximize oxygenation.
Within the first 7 days postoperatively, we focused particularly on evaluating, tracking and recording postoperative pulmonary complications, such as respiratory failure requiring intubation and mechanical ventilation, pneumonia as defined by the European Perioperative Clinical Outcome (EPCO) criteria, and atelectasis. A decrease in peripheral oxygen saturation (SpO2) to less than 90%, as determined by pulse oximetry with a FiO2 of 0.5, was referred to as hypoxemia. We assessed pulmonary problems using clinical and radiological results.
In order to reduce the risk of unfavorable outcomes, this study sought to improve the preoperative and perioperative care of patients undergoing thoracic surgery by identifying characteristics linked to a higher incidence of complications.
Results
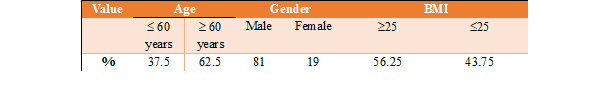
The study included 80 patients. The characteristics of the cohort are presented in Table 1. The percentage difference between genders was statistically significant and a significant association was observed between gender and lung malignancy at p<0.05. Male gender increased the likelihood of developing lung malignancy by four times (OR=4.333, 95% CI [2.12577–8.8337]). The average age of all participants was 62.9±8.2 years, ranging from 41 to 80 years. A total of 64.0% of participants were older than 64 years. The average age among male participants was 63.1±8.1 years, while the average age among female participants was slightly lower at 61.7±9.0 years.
The difference in mean values between genders was not statistically significant (p>0.05). The percentage difference between the two BMI groups was not statistically significant as well (p>0.05).
Table 1. Characteristics of the cohort.
| Value | Age | Gender | BMI | |||
| £ 60 years | ³ 60 years | Male | Female | ³25 | £25 | |
| % | 37.5 | 62.5 | 81 | 19 | 56.25 | 43.75 |
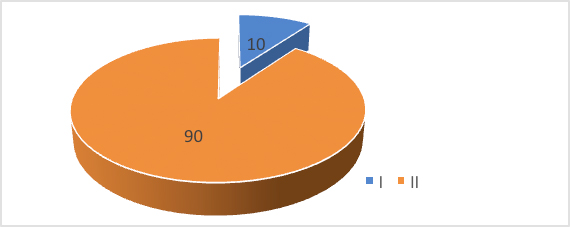
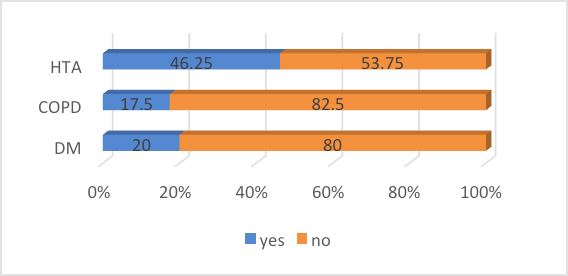
We also analyzed the distribution of patients according to the ASA classification and comorbidities presented in Figure 1 and 2.
Figure 1. Graphical representation of the percentage distribution of ASA classifications.
Figure 2. Graphical representation of the percentage distribution of diabetes mellitus (DM), hypertension (HTN) and chronic obstructive pulmonary disease (COPD).
Table 2 presents the characteristics of both the type of surgery and the surgical side. The percentage difference between lobectomy and other types of surgery is significant at p<0.05. The right side was affected in significantly higher percentage, with a significant difference at p<0.05. The average duration of single-lung collapse during surgery was 125.9±54.7 minutes, ranging from 20 to 285 minutes. In 50% of the patients, the duration of single-lung collapse during surgery exceeded 120 minutes, with a median of 120 minutes and an interquartile range (IQR) of 100–150 minutes.
Table 2. Characteristics of the surgery.
| Surgery | No | % | No | % | ||||
| Lobectomy | 38 | 67.8 | 19 | 79.2 | ||||
| Pneumonectomy | 11 | 19.6 | 0 | 0 | ||||
| Bilobectomy | 4 | 7.1 | 3 | 12.5 | ||||
| Segmentectomy | 3 | 5.4 | 2 | 8.3 | ||||
| Side of surgery | ||||||||
| Right | 32 | 57.2 | 15 | 62.5 | ||||
| Left | 24 | 42.8 | 9 | 37.5 | ||||
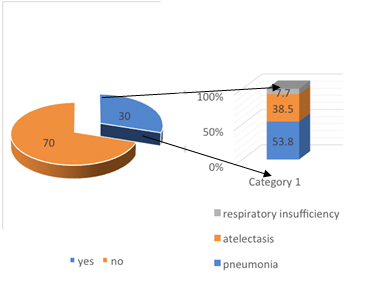
The incidence of postoperative pulmonary complications in thoracic interventions with OLV in this study was 30.0%. The occurrence of complications, including atelectasis, pneumonia and postoperative respiratory insufficiency requiring mechanical ventilation, was observed in 30.0% of the patients, while 70.0% of the patients showed no complications. The percentage difference between patients with and without complications is significant at p<0.05 (Figure 3.).
Figure 3. A graphical representation of the occurrence of complications and their types.
The percentage difference observed between pneumonia and atelectasis versus respiratory insufficiency is significant for p<0.05. The profile of patients experiencing postoperative complications during thoracic interventions with one-lung ventilation is significantly skewed towards males (87.5%) compared to females (12.5%), with a statistically significant difference of p<0.05. Postoperative pulmonary complications during thoracic interventions with OLV are observed in 75.0% of the patients aged over 60 years. The percentage difference compared to patients under 60 years old is statistically significant for p<0.05. Patients with complications have a mean age of 65.7±8.1 years. Complications are significantly more common in 79.2% of the patients who underwent lobectomy compared to other types of surgery. Among patients with complications, 65.4% had FEV₁% and FVC% values greater than or equal to 70. SpO2 % values were below 90 in 32.3% of the patients with complications, and 91.1% were smokers. An association was observed between the occurrence of complications and BMI (normal vs. overweight) for p<0.05. A higher BMI above 25 (overweight) increases the likelihood of complications during thoracic interventions with one-lung ventilation by three times (OR=3.0, 95% CI [1.1138–9.0804]). For the other variables – gender, age, type of surgery, side, ASA classification, SpO2%, smoking, diabetes mellitus, COPD, hypertension and duration of lung collapse, no significant associations with the occurrence of complications were observed for p>0.05 in this group of patients.
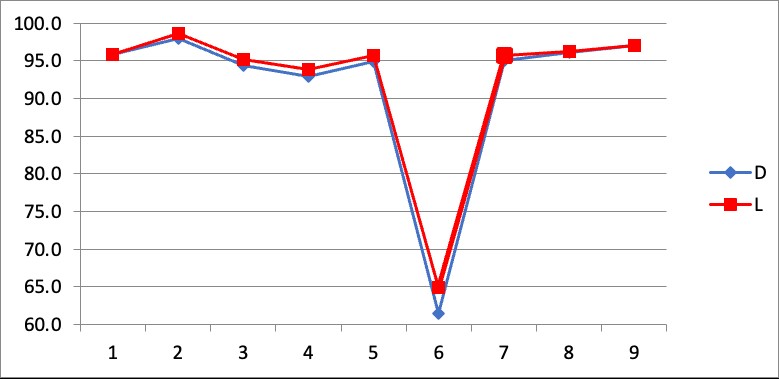
Figure 4 presents the results we obtained for the oxygen saturation in our cohort of patients. A nonsignificant greater drop in oxygen saturation was observed during right-sided operations compared to left-sided ones. The values of oxygen saturation (SpO₂%) were lower on the right sided surgeries (P<0.05).
Figure 4. Line diagram of average SpO₂% values by side of the surgery.
*D – right, L – left.
Discussion
In our study, we observed a postoperative pulmonary complication (PPC) rate of 30.0%, aligning closely with findings reported in previous literature. The most common complications in our cohort were pneumonia (17.5%) and atelectasis (12.5%), with respiratory failure, necessitating mechanical ventilation, occurring in 2.5% of the patients. These findings emphasize the critical nature of PPC as significant contributors to postoperative morbidity. In one of the largest multicenter randomized clinical trials, 1,170 patients scheduled for lung resection were included, focusing, among other things, on postoperative complications depending on the type of ventilation (10,11). Pulmonary complications were reported in 40.5% to 42.8% of the patients, depending on the ventilation parameters. This is a higher incidence than observed in our study; however, Park et al. also considered hypoxemia (SpO₂ <90%) and empyema as postoperative complications, which were not included in our study (12). The higher reported incidence may also be attributed to differences in patients’ demographics, surgical techniques, or intraoperative ventilation strategies employed across the two studies.
In the study by Fernandez et al., which analyzed 189 patients after lung resection (13), the incidence of PPC was reported at 34.3%, with pneumonia being the dominant complication, affecting 29.7% of the patients. This aligns with findings that pneumonia often represents the leading cause of morbidity following thoracic surgeries due to altered lung mechanics, immunosuppression and impaired mucociliary clearance in the postoperative period. François and colleagues, in a study involving 266 patients, reported a slightly lower incidence of postoperative pulmonary complications, documented at 25% (14). This variation in incidence highlights the importance of standardized definitions and methodologies when assessing postoperative outcomes in thoracic surgery.
In our study, the incidence of postoperative pulmonary complications was 30.0%, aligning with previous studies. The postoperative complications analyzed in our study included atelectasis, pneumonia and respiratory failure (i.e., the need for mechanical ventilation), defined according to EPCO criteria (15). Consistent with the study by Fernandez et al., our findings show that pneumonia is the most common complication following lung surgery. In our cohort, pneumonia occurred in 17.5% of the patients, which aligns with data from the literature (16-18). This finding underscores the critical need for early recognition and management of pneumonia to improve postoperative outcomes, especially in high-risk patient groups.
Atelectasis was observed in 12.5% of patients in our study. This complication, although common, is often transient and resolves with appropriate postoperative care, including physiotherapy and respiratory support. However, persistent atelectasis can significantly impact postoperative recovery, particularly in patients with pre-existing pulmonary conditions or obesity (19). Development of atelectasis has been reported as one of the most frequent respiratory complications during the perioperative period, affecting nearly 90% of the patients (20,21). The persistence of atelectasis beyond the immediate postoperative phase may exacerbate local inflammation, impair gas exchange, and predispose patients to secondary infections, including pneumonia (22). Preventive strategies, such as the use of recruitment maneuvers, optimal intraoperative ventilation and early postoperative mobilization, remain crucial in minimizing the incidence and severity of atelectasis.
Respiratory failure, defined as the need for mechanical ventilation postoperatively, was noted in 2.5% of our patients. While less common than other complications, respiratory failure is associated with significant morbidity and prolonged hospitalization. Factors contributing to respiratory failure include inadequate pulmonary reserve, prolonged surgical duration, and intraoperative events such as hypoxia or hemodynamic instability. Identifying at-risk patients preoperatively and optimizing their condition can play a pivotal role in reducing this complication.
In literature, the incidence of PPC after lung resection varies widely across studies. Differences in patients’ selection, comorbidities, surgical techniques and perioperative management likely contribute to this variability. For instance, studies utilizing advanced surgical techniques such as video-assisted thoracoscopic surgery (VATS) often report lower complication rates compared to traditional open thoracotomy approaches (23-27). Similarly, enhanced recovery protocols, including early ambulation and improved pain management, have been shown to mitigate the risk of PPC. Nonetheless, there is consensus that these complications are common.
Most of the studies agree that patients undergoing lung surgery often are presented with high burden of comorbidities during preoperative preparation, contributing to the elevated risk of postoperative pulmonary complications (24,28,29). Common comorbidities such as chronic obstructive pulmonary disease (COPD), diabetes mellitus and cardiovascular disease are known to increase susceptibility to PPC by reducing baseline pulmonary reserve and compromising immune function. Addressing these comorbidities through multidisciplinary preoperative assessment and tailored perioperative care is essential to improve surgical outcomes.
Finally, while variations in reported incidence rates exist, these studies underscore the importance of a comprehensive approach to the prevention, early detection and management of PPC in thoracic surgery. Future research should aim to harmonize definitions and methodologies to enable meaningful comparisons and develop evidence-based guidelines to optimize patient care.
Conclusion
Pulmonary complications are highly prevalent after thoracic surgery, primarily due to the physiological challenges introduced during the procedure and the use of one-lung ventilation. These challenges include significant alterations in respiratory mechanics, reduced lung compliance and ventilation-perfusion mismatch, all of which contribute to impaired gas exchange. The combination of surgical stress, anesthesia and mechanical ventilation further exacerbates the risk of complications. Effective perioperative strategies are essential to minimize these risks. Tailoring these interventions to the individual patient’s risk profile can significantly enhance outcomes and reduce morbidity associated with thoracic surgery. By implementing a comprehensive and multidisciplinary approach to patient management, healthcare teams can mitigate the incidence and severity of pulmonary complications, thereby improving recovery and reducing hospital stay duration.
References:
- Slinger P, Darling G. Preanesthetic assessment for thoracic surgery. In: Slinger P, ed. Principles and Practice of Anesthesia for Thoracic Surgery. Melbourne: Springer; 2011:11-34.
- Canet J, Gallart L, Gomar C, et al. Prediction of postoperative pulmonary complications in a population-based surgical cohort. Anesthesiology 2010; 113:1338-1350.
- Allen MS, Darling GE, Pechet TT, et al. Morbidity and mortality of major pulmonary resections in patients with early- stage lung cancer: initial results of the randomized, prospective ACOSOG Z0030 trial. Ann Thorac Surg 2006;81:1013-1020.
- Canet J, Gallart L. Predicting postoperative pulmonary complications in the general population. Curr Opin Anaesthesiol 2013; 26:107-115.
- Shelley, B.G.; McCall, P.J.; Glass, A.; Orzechowska, I.; Klein, A.A.; Association of Cardiothoracic Anaesthesia and collaborators. Association between Anaesthetic Technique and Unplanned Admission to Intensive Care after Thoracic Lung Resection Surgery: The Second Association of Cardiothoracic Anaesthesia and Critical Care (ACTACC) National Audit. Anaesthesia 2019, 74,1121–1129.
- Sen, S.; Sen, S.; Sentürk, E.; Kuman, N.K. Postresectional Lung Injury in Thoracic Surgery Pre and Intraoperative Risk Factors: A Retrospective Clinical Study of a Hundred Forty-Three Cases. J. Cardiothorac. Surg. 2010, 5, 62.
- Traibi, A.; Grigoroiu, M.; Boulitrop, C.; Urena, A.; Masuet-Aumatell, C.; Brian, E.; Stern, J.-B.; Zaimi, R.; Gossot, D. Predictive Factors for Complications of Anatomical Pulmonary Segmentectomies. Interact. Cardiovasc. Thorac. Surg. 2013, 17, 838–844.
- Khemani RG, Thomas NJ, Venkatachalam V (2012) Comparison of SpO2 to PaO2 based markers of lung disease severity for children with acute lung injury. Crit Care Med 40: 1309-1316.
- Jammer, I.; Wickboldt, N.; Sander, M.; Smith, A.; Schultz, M.J.; Pelosi, P.; Leva, B.; Rhodes, A.; Hoeft, A.; Walder, B.; et al. Standards for Definitions and Use of Outcome Measures for Clinical Effectiveness Research in Perioperative Medicine: European Perioperative Clinical Outcome (EPCO) Definitions: A Statement from the ESA-ESICM Joint Taskforce on Perioperative Outcome Measures. Eur. J. Anaesthesiol. 2015, 32, 88–105.
- Raphael J, Chae A, Feng X, Shotwell MS, Mazzeffi MA, Bollen BA, Pfeil D, Feduska E, Shah AS, Kertai MD. Red Blood Cell Transfusion and Pulmonary Complications: The Society of Thoracic Surgeons Adult Cardiac Surgery Database Analysis. Ann Thorac Surg. 2024 Apr;117(4):839-846.
- Gavrilovska-Brzanov A., Slaninka Miceska M.,Shosholcheva M., Kuzmanovska B., Kartalov A., Mojsova-Mijovska M., Jovanovski-Srceva M., Simeonov R., Brzanov N. “Carboxyhemoglobin and Methemoglobin as Markers of Postoperative Pulmonary Complications“.Journal of Anesthesia and Surgery 2018 May; 5(1): 61- 67.
- Park M. et al Driving pressure-guided ventilation and postoperative pulmonary complications in thoracic surgery: A multicenter randomized clinical trial. Br J Anaesth 2023;130:e106–18.
- Fernandes EO, Teixeira C, da Silva LCC. Thoracic surgery: Risk factors for postoperative complications of lung resection. Rev Assoc Med Bras. 2011;57:292-298.
- Stephan F, Boucheseiche S, Hollande J, Flahault A, Cheffi A, Bazelly, Bernard et al. Pulmonary complications following lung resection. A comprehensive analysis of incidence and possible risk factors. Chest. 2000;118:1-8.
- Jammer, I.; Wickboldt, N.; Sander, M.; Smith, A.; Schultz, M.J.; Pelosi, P.; Leva, B.; Rhodes, A.; Hoeft, A.; Walder, B.; et al. Standards for Definitions and Use of Outcome Measures for Clinical Effectiveness Research in Perioperative Medicine: European Perioperative Clinical Outcome (EPCO) Definitions: A Statement from the ESA-ESICM Joint Taskforce on Perioperative Outcome Measures. Eur. J. Anaesthesiol. 2015, 32, 88–105.
- Marshall C, Marshall B: Site and sensitivity for stimulation of hypoxic pulmonary vasoconstriction. J Appl Physiol 1983; 55:711– 6.
- Baar W, Semmelmann A, KnoerleinJ , Weber F, Heinrich, S, Loop T. Risk Factors for Postoperative Pulmonary Complications Leading to Increased In-Hospital Mortality in Patients Undergoing Thoracotomy for Primary Lung Cancer Resection: A Multicentre Retrospective Cohort Study of the German Thorax Registry. J.Clin.Med.2022:1;774.
- Fernandes EO, Teixeira C, da Silva LCC. Thoracic surgery: Risk factors for postoperative complications of lung resection. Rev Assoc Med Bras. 2011;57:292-298.
- Adde FV, Campos SV, Henrique R, Braga DO, Rodrigues JC. Indications for lung resection surgery and lung transplant in South American children with cystic fibrosis. Paediatr Respir Rev. 2017;25:37-42.
- Brooks-Brunn JA. Postoperative atelectasis and pneumonia: Risk factors. Am J Crit Care. 1995;4:340-9.
- Duggan M, Kavanagh BP. Pulmonary atelectasis: A pathogenic perioperative entity. Anesthesiology. 2005;102:838-54.
- Retamal J, Bergamini BC, Carvalho AR, et al. Non-Lobar atelectasis generates inflammation and structural alveolar injury in the surrounding healthy tissues during mechanical ventilation. Crit Care 2014;18:505.
- Brunelli A, Anthony WK, Kenneth IB, et al. Physiologic evaluation of the patient with lung cancer being considered for resectional surgery: diagnosis and management of lung cancer, 3rd ed: American College of Chest Physicians evidence-based clinical practice guidelines. Chest. 2013:143:166-190.
- Hurford WE, Kolker AC, Strauss HW. The use of ventilation/ perfusion lung scans to predict oxygenation during one-lung anesthesia. Anesthesiology. 1987;67(5):841–4.
- Marshall C, Marshall B: Site and sensitivity for stimulation of hypoxic pulmonary vasoconstriction. J Appl Physiol 1983; 55:711– 6.
- Hambraeus-Jonzon K, Bindslev L, Mellgård AJ, Hedenstierna G: Hypoxic pulmonary vasoconstriction in human lungs. A stimulus-response study. Anesthesiology 1997; 86:308 –15.
- Boffa DJ, Allen MS, Grab JD, Gaissert HA, Harpole DH, Wright CD. Data from The Society of Thoracic Surgeons General Thoracic Surgery database: the surgical management of primary lung tumors. J Thorac Cardiovasc Surg. 2008;135(2):247-54.
- Steier J, Lunt A, Hart N, Polkey MI, Moxham J. Observational study of the effect of obesity on lung volumes. Thorax. 2014;69(8):752–912.
- Guenoun T, Journois D, Silleran-Chassany J, Frappier J, D’attellis N, Salem A, Safran D: Prediction of arterial oxygen tension during one-lung ventilation: Analysis of preoperative and intraoperative variables. J Cardiothorac Vasc Anesth 2002; 16:199 –203.