UDK: 616.12-073.432.19:616-089.5
Naumovski F., Shosholcheva M., Jovanovski-Srceva M., Nancheva J., Durnev V., Ognjanova V.
University Clinic for Traumatology, Orthopedics, Anesthesiology, Reanimation, Intensive Care and Emergency Center – Skopje, Department of Anesthesiology, Reanimation and Intensive Care
Abstract
Both procedures, transthoracic echocardiography (TTE), as well as transesophageal echocardiography (TEE), in the anesthesiologist’s hands could be considered as a must in providing significant data about the hemodynamics while following the beat-to-beat dynamical circulatory changes. Echocardiography as a noninvasive procedure is a real time provider of information about the systolic and diastolic function, valvular structures, fluid status, ventricular contractility and the cardiac output in perioperative setting, as well in critically ill patients. The intention of this article is to elaborate the basic echocardiographic findings which imply the fluid status referred as “The tank”, cardiac contractility named as “The pump” and significant findings that involve the pericardium referred as “The surroundings” with the idea of providing the anesthesiologists with enough knowledge to perform basic echocardiographic examination to rule out existence of significant life-threatening conditions in order to provide better patient care while managing complex cases. Here we offer only brief information about the power of echocardiography with the idea to encourage anesthesiologists to start using it as a monitoring tool on a daily basis in a well-selected cases. Detailed and more precise echocardiographic examination is beyond the scope of this article and should be considered for physicians who already pose basic echocardiographic skills.
Key Words: Echocardiography; Point of Care Ultrasound; Transthoracic Echocardiography.
Introduction
Modern anesthesiologists and intensivists tend to move borders between specialties in order to provide more accurate patient’s care when making prompt decisions on a daily basis. Many years ago, performing perioperative echocardiography as a point of care method, was considered as a procedure which was beyond the anesthesiologist’s responsibilities. Rather than that, nowadays, both procedures – transthoracic echocardiography (TTE), as well as transesophageal echocardiography (TEE) in the anesthesiologist’s hands could be considered as a must providing significant data about the hemodynamics while following the beat-to-beat dynamical circulatory changes. According to the observational study done by Brian Cowie where performing echocardiography by anesthesiologists was examined, in 98% of the cases the anesthesiologists have obtained a high-quality image for analysis and in 84% of the cases this examination has led to change in therapy in the perioperative period [1]. Echocardiographic findings stated by the anesthesiologists corelated with those when echocardiography was performed by cardiologist in an 87% of the cases [1] which could be considered as an even bigger reason why should echocardiography be part of the standard monitoring in the perioperative period. Echocardiography as a noninvasive procedure is a real time provider of information about the systolic and diastolic function, valvular structures, fluid status, ventricular contractility and the cardiac output [2] in perioperative setting, as well in the critically ill patients. All above mentioned data could lead to significant changes while managing patients with previously established diagnosis of coronary artery disease or stable chronic heart failure who could easily deteriorate perioperatively [2].
In this article we will elaborate the basic echocardiographic findings which imply the fluid status referred as “The tank”, cardiac contractility named as “The pump” and significant findings that involve the pericardium referred as “The surroundings” with the idea of providing the anesthesiologists with enough knowledge to perform basic echocardiographic examination to rule out existence of significant life threatening conditions in order to provide better patient’s care while managing complex cases. Echocardiographic examination done by intensivists as a point of care tool while monitoring patients in order to assess volume status, myocardial contractility and to detect life threatening conditions was strongly advised and encouraged by the European Society of Intensive Care Medicine and published back in 2021 [3].
The Tank
Many conditions even in elective patients could result in hypotension and one of them is hypovolemia. Hypovolemia is more frequently met in non-elective emergent cases, where performing TTE could reveal the reason of hypotension and to help us while guiding therapy, when giving volume boluses till reaching homeostasis. There are many static and dynamic ways to assess the volume status and volume responsiveness, but in this article, we will discuss the simplest echocardiographic approaches of volume status assessment, in order to provide the reader with knowledge for gaining simple and basic echocardiographic skills. The quickest and the simplest way to rule out does the reason for hypotension could be hypovolemia, is when we take a look at the heart in parasternal long axis where the left ventricle and Left Ventricular Outflow Tract are seen. Actually in severely hypovolemic patients the heart structures will be looking hyperkinetic, which means left ventricular free wall and interventricular septum will move inwards meeting and “kissing” one another inside the empty ventricle. This sign of a kissing ventricle suggests serious hypovolemia and demands aggressive fluid resuscitation. In situations where hypovolemia is not that severe left ventricular wall movements would be still hyperkinetic but more subtle and not so reliable for diagnosis. In those situations, especially in spontaneously breathing patients, the anesthesiologist must take a look at the Inferior Vena Cava (IVC) diameter and its collapsibility. By placing the probe in the subcostal area, we could find the IVC and see how it enters the right heart. The best place to measure the IVC diameter and evaluate the dynamic changes over respiratory cycle is at 2-3cm before entering the right heart. Measuring IVC over time is possible in M-mode where the movements or venous collapse will be registered. Normal values for the maximal IVC diameter are considered from 12mm to 21mm, where all values below 12mm could suggest hypovolemia [4]. Patients could have normal values for maximal IVC diameter and still be hypovolemic which could be demystified with simple measuring the largest and the smallest diameter of IVC in M-mode during the respiratory cycle in spontaneously breathing patients, as well as in mechanically ventilated patients. In spontaneously breathing patients we should measure IVC collapsibility index using the following formula: dIVCmax-dIVCmin/dIVCmax x100, while in mechanically ventilated patients we should look for IVC distensibility index calculated by the following formula – dIVCmax-dIVCmin/dIVCmin x100. The difference in calculating IVC collapsibility versus distensibility lays in the different physiology of respiration among spontaneously breathing patients versus mechanically ventilated patients. In spontaneously breathing patients IVC collapses during inspiration, because of the negative intrathoracic pressures which facilitate the emptying the IVC into the right atrium. In mechanically ventilated patients due to positive end expiratory pressure during inspiration, IVC dilates. Measuring above mentioned diameters and indexes in seconds could provide us information about the fluid responsiveness of our patients making significant contribution to the diagnosis of the reason of hypotension, but as well in guiding therapy. Therefore, as a bigger the difference of IVC diameter over the respiratory or ventilatory cycle is, the bigger is the volume responsiveness suggesting hypovolemia. IVC collapsibility index has sensitivity of 71% and specificity of 81% in terms of predicting volume responsiveness in spontaneously breathing patients according to 7 studies which had evaluated a total of 395 patients [5]. Sensitivity and specificity of IVC distensibility index when predicting volume responsiveness in mechanically ventilated patients is quite similar with 75% and 82% respectively, based on 9 studies which have included 284 patients [5]. Blood loss even at 500ml was accompanied with lowering the diameter of IVC for 33-40% from baseline values before the physiological changes of vital signs, as hypotension and tachycardia occur [6]. Therefore, dimensions of IVC less than 21mm with IVC collapsibility index greater than 50% in spontaneously breathing patients could suggest slight hypovolemia, but dimensions of IVC lower than 18mm combined with collapsibility index greater than 50% strongly suggest hypovolemia and fluid responsiveness. In mechanically ventilated patients IVC distensibility index greater than 18% implies hypovolemia and fluid responsiveness. However, even more accurate and precise echocardiographic methods for assessment of volume status are available nowadays as measuring the Left Ventricular Outflow Tract Velocity Time Integral with Cardiac output measurement and transmittal flow velocity measurement, but they are considered beyond the basic echocardiographic skills and will not be discussed in this article.
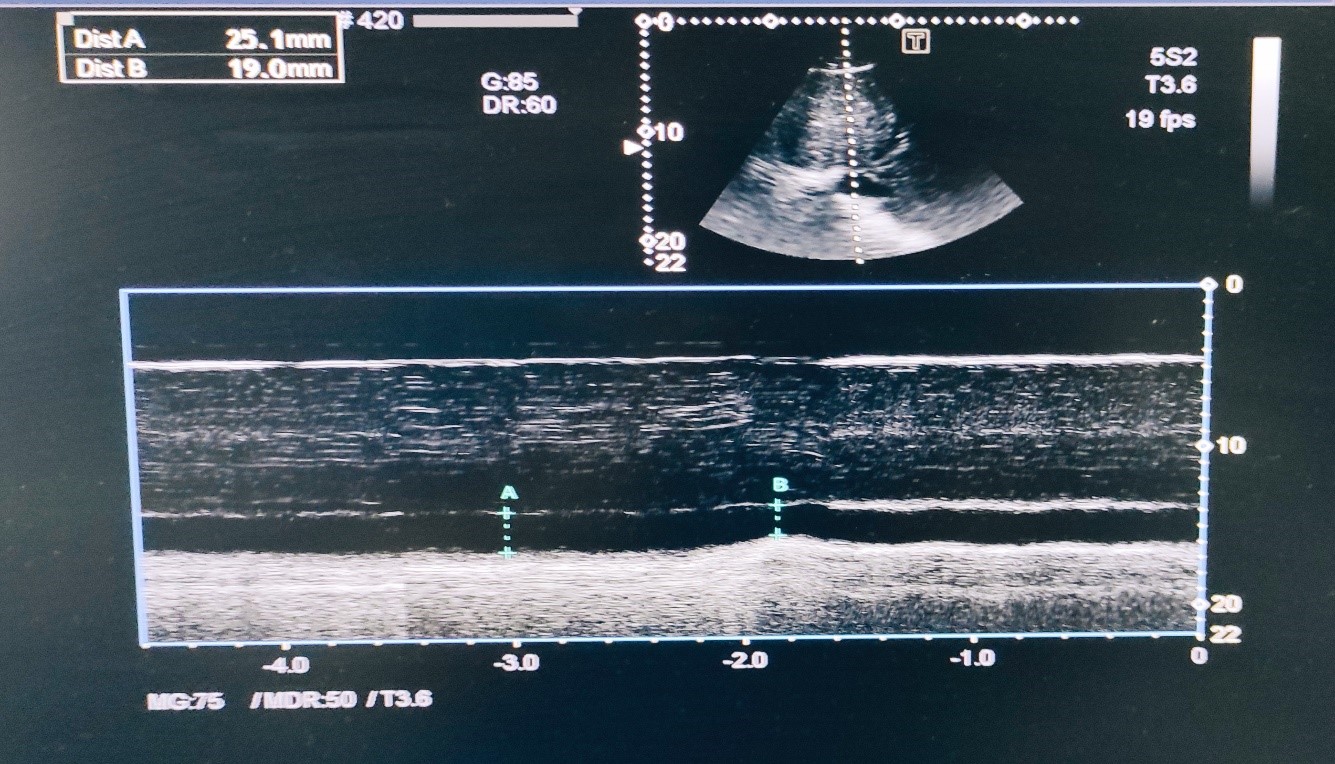
Figure 1. M-mode of dilated Inferior Vena Cava with collapsibility less than 50%.
The pump
The assessment of cardiac function, precisely the cardiac contractility, is frequently needed before surgery or in shocked patients admitted in the ICU. Elective patients could undergo detailed echocardiographic examination done by cardiologist, but in terms of emergence in complex cases before emergent surgery or during the ICU stay due to resolving acute onset situations, sometimes cardiac contractility should be assessed by the anesthesiologist. Measuring ejection fraction as a surrogate of a cardiac contractility is a mainstay in assessment of cardiac function in elective patients, but it is not a reliable method in shocked patients because ejection fraction is preload and afterload dependent [7]. Therefore, other methods should be used when assessing cardiac function in critically ill patients. As a basic skill, the anesthesiologist who will perform point-of-care ultrasound (POCUS), in order to provide quick solution in a deteriorating patient, should use simple eyeballing while assessing cardiac contractility. Nevertheless, eyeballing by itself is not as precise nor objective as expected, but still could help in revealing does cardiac contractility is acutely affected. Eyeballing should be done in parasternal long axis and four chamber view. In parasternal long axis view, one should look after the movements of the left ventricular wall towards the septum, as well as the movement of the mitral valve during opening. Actually if the left ventricular wall moves fine towards the septum and mitral valve while maximally opened is placed near the septum, global cardiac contractility is considered as preserved. When movements of the left ventricular wall are flattened and not easily visible, as well as when the mitral valve during maximally opening is far from the myocardial septum pump, insufficiency should be considered as a significant contributor to the hemodynamic instability. Global systolic function estimation by eyeballing should be made in the 4-chamber apical view, as well as it is considered as a basic skill which is strongly recommended by the ESICM [3]. Throughout this window, the left ventricle is better visualized from the apex to the base where radial and longitudinal shortening could be seen and assessed during systole. Based on the simple eyeballing, we could make a conclusion if the cardiac contractility is increased, normal, mildly or severely impaired which in most of the cases could lead to significant changes in therapeutic approach. Increased cardiac contractility in most of the critically ill patients suggests hypovolemia with consequently strongly activated sympathetic response while impaired contractility could be the cause or sometimes even a consequence of the critical illness.
The Surroundings
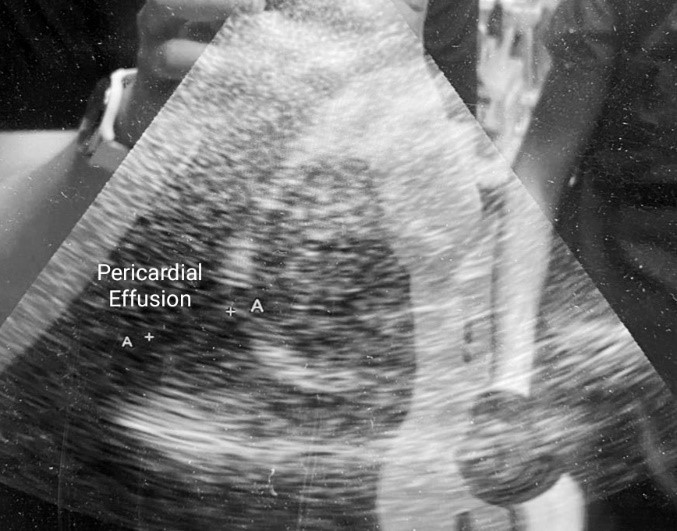
The most significant condition with a life-threatening property that must not be missed when performing POCUS, is pericardial tamponade. “The surroundings” refers to pericardium and the structures around the heart whose pathologic conditions could lead to impaired hemodynamics. Accumulation of free fluid between the two pericardial layers could be detected in all cardiac windows where pericardial effusion will be visualized as a dark anechoic area around the heart whose dimensions could vary depending on the amount of pericardial fluid [8]. In emergent cases where time to treatment is crucial, even only subcostal examination could reveal presence of pericardial effusion with or without hemodynamic compromise leading to fast treatment decision. If the anechoic dark space could be seen in all windows around the heart, then the pericardial effusion is probably big. Essential when deciding if pericardiocentesis is needed or not, is the presence or absence of hemodynamic compromise which by echocardiographic could be identified by detecting collapse of the right atrium in systole or right ventricular collapse in diastole. Right heart collapse could be identified when using subcostal or apical 4-chamber view during the examination where inward movement of the right ventricular free wall is met during diastole. Pericardial tamponade in 92% of the cases is accompanied with dilation of the IVC [8] which becomes larger than 2.5cm and non-collapsible implying impaired anterograde blood flow and should be seen and assessed in subcostal view as it was explained earlier in this article.
Figures 2 & 3. Pericardial Effusion surrounding the heart.
Conclusion
Point of Care Echocardiography in the Anesthesiologists hands when adequately indicated and performed could lead to significantly faster diagnosis of life-threatening conditions demanding immediate treatment. The assessment of the heart function perioperatively by echocardiography should be treated as one more window available to look at the hemodynamics. Echocardiography, even when performed by the very basic skilled Anesthesiologist-Echocardiographer in states of hemodynamic instability could provide answers about the volume status, heart contractility and possible obstructive etiology leading us to decisions based on findings, but rather on assumption while providing the safest possible care for patients.
References:
- Cowie B. Focused cardiovascular ultrasound performed by anesthesiologists in the perioperative period: feasible and alters patient management. J Cardiothorac Vasc Anesth. 2009 Aug;23(4):450-6. doi: 10.1053/j.jvca.2009.01.018.
- Manecke GR Jr, Vezina DP. Perioperative transthoracic echocardiography: “universal acid”? J Cardiothorac Vasc Anesth. 2009 Aug;23(4):447-9. doi: 10.1053/j.jvca.2009.05.024.
- Robba C, Wong A, Poole D, Al Tayar A, Arntfield RT, Chew MS, Corradi F, Douflé G, Goffi A, Lamperti M, Mayo P, Messina A, Mongodi S, Narasimhan M, Puppo C, Sarwal A, Slama M, Taccone FS, Vignon P, Vieillard-Baron A; European Society of Intensive Care Medicine task force for critical care ultrasonography*. Basic ultrasound head-to-toe skills for intensivists in the general and neuro intensive care unit population: consensus and expert recommendations of the European Society of Intensive Care Medicine. Intensive Care Med. 2021 Dec;47(12):1347-1367. doi: 10.1007/s00134-021-06486-z. Epub 2021 Oct 5. PMID: 34787687; PMCID: PMC8596353.
- Porter TR, Shillcutt SK, Adams MS, Desjardins G, Glas KE, Olson JJ, Troughton RW. Guidelines for the use of echocardiography as a monitor for therapeutic intervention in adults: a report from the American Society of Echocardiography. J Am Soc Echocardiogr. 2015 Jan;28(1):40-56. doi: 10.1016/j.echo.2014.09.009. PMID: 25559474.
- Kaptein MJ, Kaptein EM. Inferior Vena Cava Collapsibility Index: Clinical Validation and Application for Assessment of Relative Intravascular Volume. Adv Chronic Kidney Dis. 2021 May;28(3):218-226. doi: 10.1053/j.ackd.2021.02.003. PMID: 34906306.
- Johnson BD, Schlader ZJ, Schaake MW, O’Leary MC, Hostler D, Lin H, St James E, Lema PC, Bola A, Clemency BM. Inferior Vena Cava Diameter is an Early Marker of Central Hypovolemia during Simulated Blood Loss. Prehosp Emerg Care. 2021 May-Jun;25(3):341-346. doi: 10.1080/10903127.2020.1778823. Epub 2020 Jul 7. PMID: 32628063; PMCID: PMC8672380.
- Zerbib Y, Maizel J, Slama M. Echocardiographic assessment of left ventricular function. J Emerg Crit Care Med 2019; 3:33.
- Pérez-Casares A, Cesar S, Brunet-Garcia L, Sanchez-de-Toledo J. Echocardiographic Evaluation of Pericardial Effusion and Cardiac Tamponade. Front Pediatr. 2017 Apr 24;5:79. doi: 10.3389/fped.2017.00079. PMID: 28484689; PMCID: PMC5401877.