Brzanov N1, Labacevski N2, Antovik S3, Trpevski S1, Ognjenovic Lj3, Gavrilovska –Brzanov A1
1University Clinic for Traumatology, Orthopedic Diseases, Anesthesia, Reanimation, Intensive Care and Emergency Centre, Medical Faculty, University “Ss. Cyril and Methodius,” Skopje, Macedonia
2Department of Preclinical and Clinical Pharmacology and Toxicology, Faculty of Medicine, University “Ss. Cyril and Methodius”, Skopje, Macedonia
3Uniersity Clinic for Abdominal surgery, Medical Faculty, University “Ss. Cyril and Methodius,” Skopje, Macedonia
DOI: https://www.doi.org/10.55302/MJA2373054b
Abstract
Introduction: This article discusses the importance of trauma assessment in healthcare settings and the role of focused assessment with sonography in trauma (FAST) scans as a diagnostic tool. Trauma remains a significant health concern worldwide, leading to high mortality and morbidity rates, particularly in the younger population. Identifying risk factors for death is crucial for improving trauma patient’s outcomes.
Objective: The objective of the study is to implement FAST assessments in an inner-city emergency department and examine their impact on the treatment of adult trauma patients.
Material and Methods: The study took place in an urban trauma center and included patients over 18 years old who were presented with trauma, excluding pregnant females, unstable patients and those without consent. FAST scans were performed using ultrasound machines, assessing various abdominal and thoracic views.
Results: The results revealed a high sensitivity of 94.4% and a specificity of 85.71% for FAST scans, making them a valuable tool for detecting abdominal free fluid in trauma patients.
The most of trauma patients in the study were men aged between 25 and 55, with falls, traffic accidents and assaults being the primary causes of blunt trauma. Commonly affected organs included the lungs, liver and spleen. FAST scans were found to be particularly useful for hypotensive patients, helping in triage decisions. While FAST scans demonstrated high sensitivity and specificity, the study suggests that patients with negative results should be observed and may benefit from follow-up scans, as small amounts of free fluid can be challenging to detect.
Conclusion: In conclusion, FAST scanning offers several advantages as a diagnostic tool for trauma assessment including its accessibility, affordability, repeatability, noninvasiveness and quick setup. It complements traditional methods like CT scans, especially in cases of hypotensive patients. Despite their limitations, FAST scans play a significant role in improving the management of trauma patients, helping healthcare professionals to make informed decisions about patients’ care. To fully investigate the potential of FAST scans in trauma situations, additional research is required.
Key Words: diagnostic tools, emergency department, focused assessment with sonography in trauma, trauma patients.
Introduction
No matter the level of socioeconomic development, trauma is a serious health issue in every country and is still the leading cause of death in the first 40 years of life. It is also related to high morbidity and mortality (1, 2). In our country in 2021, the trauma mortality rate was 6.3 per 100,000 citizens (2).
Risk factors for death must be thoroughly identified and researched in order to reduce mortality in cases of trauma. Numerous of these risk variables, including gender, the amount of time between the injury and operation, shock at the time of admission and cerebral injuries, have been documented in research in recent years. Therefore, providing the best care for trauma patients necessitates a multidisciplinary approach. Quick identification and treatment are thought to be essential to managing the trauma patient successfully, as undetected injuries can result in avoidable fatalities (4).
Nowadays, procedures for identifying blunt trauma have been significantly altered by using Focused Assessment with Sonography in Trauma (FAST) and helical CT scans, which have also improved judgment and allowed physicians to choose patients for conservative treatment (5).
CT scans, which are noninvasive and have emerged as the gold standard for evaluating traumatic abdominal trauma, can yield incredibly precise images (6, 7). However, there are a few disadvantages and drawbacks to CT scans. The primary cause is that unstable patients are unable to use it since they have to be moved from the ER to the scanner. Specialized radiologists and radiographers are needed for the operation in order to execute the examination and interpret the images. Some individuals have reported allergic reactions after using contrast agents (8). Also, it should be remembered that the abdomen CT’s effective radiation dose is equal to 400 chest x-rays and 2.7 years’ worth of naturally occurring radiation. Yet, the danger is balanced out as follows: The potential radiation danger is outweighed by the advantage of a correct diagnosis in these severe wounds (9, 10).
FAST was the first employed in emergency rooms in the 1990s due to the necessity for a quick diagnostic method that could be applied to the situation. It is done following the primary survey to determine whether there is any free fluid in the peritoneal cavity that could be hemoperitoneum and to enable it (5). CT scanning may be recommended for hemodynamically stable patients in order to provide timely and appropriate therapy. The position and extent of the injury may not be identified in the absence of formal, complete imaging, which might substantially lengthen the time spent in the operating theater for hemodynamically unstable patients undergoing an emergency laparotomy; CTs can identify solid organ damage, unlike FAST scans. Despite FAST’s popularity, there is still uncertainty and a lack of proof about any genuine benefit to patient’s survival (2, 11, 12).
Despite the fact that there are limited prospective trials conducted in this area, this has the consequence that we are still discovering how helpful it is as a diagnostic tool and in modifying patient’s therapy (12, 13).
FAST is frequently the initial imaging test in trauma cases, which is unfortunately not applicable in our country.
Objectives
Therefore, the objective of our study was to implement this FAST assessment in our university emergency department to find out how FAST scan results can be implemented in a typical inner-city ER and whether they affect how adult trauma patients are treated afterwards.
Material and Methods
This prospective clinical observation study was conducted with the approval of the Ethics Committee and the patients’ or their guardians’ signed informed consent at the University Clinic for Traumatology, Orthopedic Diseases, Anesthesia, Reanimation, Intensive Care and Emergency Centre, Medical Faculty, University “Ss. Cyril and Methodius,” Skopje, Macedonia, in the Emergency Department, a premier trauma center in our country. All patients over the age of 18 who were presented with trauma in our department received a FAST scan when they arrived at the emergency room during the period of primary check and stabilization. Excluded were all pregnant female patients, patients who underwent urgent surgical intervention, unstable patients who were transferred to the intensive care unit, and patients without permission to participate.
After evaluation and examination according to the A, B, C, D and E standardized protocols by the attending doctor, each patient who met the inclusion criteria underwent FAST within the first 2–5 minutes of their arrival. Then, all of them were candidates for FAST as soon as possible. Patients originally underwent a FAST scan in the supine position. A FAST examination was performed using a mobile US machine with a curvilinear 3.5–5 MHz probe and a linear 5–20 MHz probe. The examiner stood to the right of the patient to obtain the following five standard views:
The pericardium was examined using the transverse view of the pericardial view, sometimes referred to as the subcostal or subxiphoid view. The most common sonographic window to the heart is the liver in the epigastric area. An alternative method that may be employed if anatomical limitations hinder the implantation of an epigastric probe is the parasternal or apical four-chamber views.
The longitudinal view of the right upper quadrant (RUQ), the Morison pouch view, or the perihepatic view are all terms for the right flank view. It displays the right kidney, right liver lobe, right paracolic gutter and the area between them (the Morison pouch). Once the hepatorenal interface, also known as the Morrison pouch, has been located, the pleural and more cephalad subphrenic spaces are evaluated. The left kidney, spleen, interstice and left paracolic gutter are seen in the longitudinal view of the left upper quadrant (LUQ). What’s commonly called the perisplenic or left upper quadrant vision gradually explores four different regions.
Transverse and longitudinal views of the suprapubic region, commonly referred to as the suprapubic view, are explored for free fluid. The bladder and rectouterina, also known as the rectrovesical pouch or the Douglas pouch, are depicted in this region, which is the most reliant peritoneal space in the supine trauma patient utilizing the bladder as a sonographic window in a transverse sweep. The probe would be positioned longitudinally along the midclavicular line at the third or fourth intercostal space in bilateral thoracic images A traumatic pneumothorax can be detected by lung sliding, which is a sensitive but non-specific indication.
All the FAST scans can be divided into four groups:
- Positive scans with pathology present (on CT),
- Positive scan but without pathology,
- Negative scan, but with pathology actually present, and
- Negative scan without pathology.
The patients’ information and details will be kept completely private.
Statistical Analysis
All the statistical analysis were done on the 20. Statistical package for social sciences. Specificity, sensitivity, and positive and negative predictive values of FAST performed by EMRs and RRs were calculated and compared using Chi-square analysis. P-value less than 0.05 was considered statistically significant.
Results
All 30 subjects in our study had experienced blunt trauma as a result of assaults (16.6%), falls (40%), or traffic accidents (43.3%). Nine women (23.2%) and 21 men (76.8%) participated in the study. A minimum age of 18 was required for the sample. The most of the participants were between the ages of 39 and 50, with a mean age of 39±17 years. As is clear from the study, the most of individuals had thoracic injury (n=15) 50% and (n=26) 86.6% had no visceral injury. These participants were followed by (n=3) 10% patients with spleen injury, (n=1) 3.3% patients who had liver injury.
The different angles from which the FAST scans were conducted while all patients were lying in supine position on the examination couch, and three points on the lung were inspected (the upper anterior point, the lower anterior point and the posterior lateral alveolar or pleural point) on each side. The abdomen was examined in three points as well. The longitudinal view of the RUQ, LUQ, showed the most dependent peritoneal space in the supine trauma patient to depict the urinary bladder and rectouterina, or rectrovesical pouch, or the pouch of Douglas and subxiphoid space. The results clearly show that the greatest percentage of FAST scans performed (n=26) revealed no free fluid (86.6%). This was followed by splenorenal views (n=2) 6.6%, hepatorenal views (n=1) 3.3%, and pelvic views (n=1) 3.3%. FAST scans on the lungs revealed pneumothorax in (n=13) 43.33% of the patients. FAST scan with pneumothorax finding is presented in Figure 1. The participants’ various organs were impacted overall by blunt injuries. The average time of the examination was 5±3.5 min. The findings showed that the following FAST scan values were attained, with a high 94.4% sensitivity. The results showed that the specificity was 85.71%, the positive predictive likelihood ratio 6.61 or positive predictive value of 3.21% and the negative likelihood ratio 0.06 or negative predictive value of 99.97%. There was not any complication to report in the exanimated cohort.
Table1. Effected organs on FAST
| Organs effected | N | % |
| Bladder | / | / |
| Kidneys | / | / |
| Liver | 1 | 3.3% |
| Lungs | 15 | 50% |
| Pancreas | / | / |
| Spleen | 3 | 10% |
Note. n=frequency, %=percentages
Table 2. Comparative of FAST with radiology findings.
| Positive pathology | Negative pathology | Total | |
| Positive FAST | 17 | 2 | 19 |
| Negative FAST | 1 | 12 | 13 |
| Total | 18 | 14 | 32 |
Table 3. Frequencies and percentages of the demographic characteristics of sample.
| FAST variable | N | % |
| Subxiphoid view | / | / |
| Right upper quadrant
(Morison pouch view) |
1 | 3.3% |
| Left upper quadrant | 2 | 6.6% |
| Suprapubic view | 1 | 3.3% |
| Bilateral thoracic views | 15 | 50% |
Note. n=frequency, %=percentages
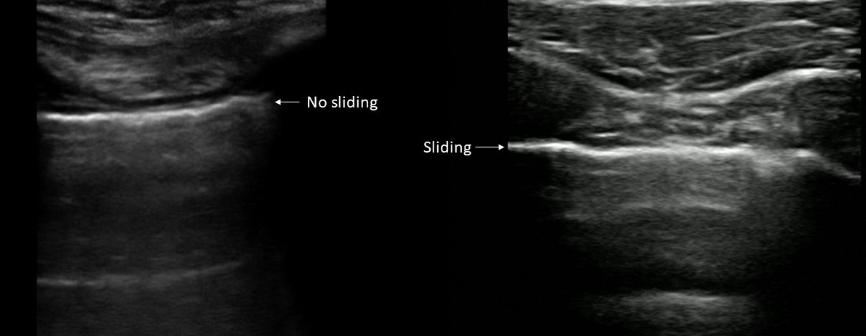
Figure 1. Thoracic views of FAST.
Discussion
In the current study, 30 victims of trauma were evaluated using FAST. The most of participants in the current study were men 21, which is consistent with earlier studies as more men participate in outdoor activities, have car accidents, and sustain other blunt injuries because few women sustain accidental wounds (14). Additionally, the most of participants in the current study were between the ages of 39 and 55. It differs from the findings of other studies where the most of participants were younger since younger people spend more time outdoors than older persons do (15). According to the study, there may have been a greater risk of harm among the patients who rode motorbikes, depending on the type of vehicle and the driver’s abilities. As these age groups tend to be dependent on other people and are not as accustomed to outdoor experiences, there were few patients who were young or old, about sixty.
Additionally, it has been noted that FAST examination is now in expansion as the only imaging method used to diagnose traumatic injuries replacing contrast CT scans. A rapid fix that can be utilized by a not expensive, small device of ultrasound during the initial survey is the FAST method to detect abdominal free fluid. Precise evaluation of people with traumatic injuries is a tough challenge for emergency doctors. While CT of the abdomen is thought to be the gold standard, it does have some disadvantages, such as high cost and time, the need to remove the patient from the ER and radiation exposure, so ultrasound can safely take its place as long as FAST exhibits high values for sensitivity and specificity (16).
The American College of Surgeons recommended FAST as an alternative to diagnostic peritoneal lavage or CT due to the historical data from studies conducted in the early years of FAST scan usage in a trauma setting, primarily during the 1990s. FAST scan was also held in such high regard that it was integrated into the Acute Trauma Life Support (ATLS) program and in Germany it was made a requirement for the surgical residency (17).
A positive result in a FAST scan should be recognized and addressed right away, according to the scan’s high Positive Predictive Value and high specificity. However, it is also wise to carefully evaluate what action should be taken that the sensitivity is 46.2% and a quarter of the results are false negative (17).
Our study shows consistency with previous studies by showing that very high values of sensitivity and specificity were obtained, 94.4% sensitivity and 85.71% specificity. CT is considered a gold standard for blunt torso trauma, but it includes shifting the patient, long time of assessment, needs of radiologist specialist availability and also exposes the patient to different types of radiations. As a result, FAST is increasingly being used in emergency departments and in trauma referral centers because of the workload in emergency, as well as radiology departments as it can easily be done on bedside. Therefore, FAST plays a major part in the classification of victims who may require more procedures for hemodynamic stabilization (15).
It was consistent with the current study because certain patients with severe injuries could not be moved for CT scanning owing to a lack of time; therefore, it was preferred to move the badly injured patients directly for treatment operations without undergoing CT scan.
To provide patients with traumatic abdominal injury with the best possible care, early diagnosis of intra-abdominal injury is essential. Although CT is still the best test for evaluating these patients, it may not be possible to do one for a variety of reasons, the most frequent of which are hemodynamic instability or pregnancy. The potential benefits and drawbacks of FAST scan versus CT scanning are evident. It is simple to perform, portable, and may be done at the patients’ bedside without exposing them to radiation. A negative scan does not always rule out an occult pathology, which may later require further intervention. It is also user dependent, as this data reveals (17).
According to research, attacks, falls and traffic accidents account for the most of cases of Blunt trauma. The most frequently injured organs in blunt abdominal trauma are the liver, spleen, visceral injuries and kidneys, which is consistent with the results of our study. The most of patients in our study had no visceral injuries (n=26), victims with spleen injuries (n=3), and victims with liver injuries (n=1), showing consistency with prior findings (18).
It is clear from the results of the current study and comparisons to earlier research conducted globally, about the diagnostic accuracy of FAST. It plays a significant role in the diagnosis of trauma patients and is being used more frequently in emergency rooms. However, it is advised to perform the CT scan of the patient after the FAST scan, if the patient is stable for confirmation of more serious injuries and more accurate results.
Chiu et al. in their study voiced legitimate questions about the sensitivity of FAST scan considering all positive studies that have been published in relation to it. According to their study, 50 out of 196 patients who had free fluid on their CT scans, had no fluid visible on their FAST scans (19). Although the data from this study was inconsequential in terms of these conclusions, Kahan et al. discovered that more than 25% of patients with visceral injuries did not have free fluid on FAST scans conducted at admission. Therefore, the use of FAST for free fluid detection does have its limitations, which physicians must consider as part of a thorough clinical examination. The number of patients who had additional intervention, regardless of their FAST result, indicated that the trauma teams are aware of these limits and the necessity for examination and reassessment (20).
In fact, it has been argued that FAST was the most beneficial in the context of hypotensive patients and that it may be used to ‘triage’ patients toward laparotomy or additional clinical assessment or investigation rather than simply diagnosing them (21-23).
It has been suggested that if a patient is clinically stable on routine reassessment, a negative FAST scan should be followed up by observation with at least a follow-up FAST scan because small amounts of free fluid are difficult to detect by FAST, even by experienced practitioners, or may not be detected at all. This issue hasn’t been the subject of any experiments (17). Serial FAST examinations weren’t used in this study. According to evidence, this practice makes FAST more sensitive (24-26).
Conclusion
FAST scanning has been incorporated into current practice because it is easily accessible, affordable, repeatable, noninvasive, and only requires a short amount of setup time. It may also be carried out using transportable equipment, giving patients more flexibility in how they are positioned, than it is feasible with other imaging modalities.
References:
- Melniker LA, Leibner E, McKenney MG, Lopez P, Briggs WM, Mancuso CA. Randomized controlled clinical trial of point-of-care, limited ultrasonography for trauma in the emergency department: the first sonography outcomes assessment program trial. Ann Emerg Med. 2006 Sep;48(3):227-35.
- Smith J. Focused assessment with sonography in trauma (FAST): should its role be reconsidered? Postgrad Med J 2010;86:285e91. doi:10.1136/ pgmj.2008.076711.
- World Health Organization. https://www.who.int/ Assessed April 04.04.02.2023.
- Radwan MM, Abu-Zidan FM. Focussed Assessment Sonograph Trauma (FAST) and CT scan in blunt abdominal trauma: surgeon’s perspective. Afr Health Sci. 2006 Sep;6(3):187-90. doi: 10.5555/afhs.2006.6.3.187.
- Fleming S, Bird R, Ratnasingham K, Sarker SJ, Walsh M, Patel B. Accuracy of FAST scan in blunt abdominal trauma in a major London trauma centre. Int J Surg. 2012;10(9):470-4. doi: 10.1016/j.ijsu.2012.05.011.
- Diercks DB, Mehrotra A, Nazarian DJ, Promes SB, Decker WW, Fesmire FM; American College of Emergency Physicians. Clinical policy: critical issues in the evaluation of adult patients presenting to the emergency department with acute blunt abdominal trauma. Ann Emerg Med.2011;57(4):387-404.doi:10.1016/j.annemergmed.2011.01.013.
- Shanmuganathan KS, Mirvis E, Sover ER. Value of contrast-enhanced CT in detecting active hemorrhage in patients with blunt abdominal or pelvic trauma. AJR Am J Roentgenol 1993;161(1):65e9.
- Brenner David J, Hall Eric J. Computed tomography d An increasing source of radiation exposure. N Engl J Med 2007;357:2277e84.
- Mettler Jr Fred A, Huda W, Yoshizumi TT, Mahesh M. Effective doses in radiology and diagnostic nuclear medicine: a catalog. Radiology July 2008;248(1):254e63.
- Soto, J.A. and Anderson, S.W. (2012). Multidetector CT of Blunt Abdominal Trauma. Radiology, 265(3), pp.678–693.
- Kornezos, I., Chatziioannou, A., Kokkonouzis, I., et al. (2009). Findings and limitations of focused ultrasound as a possible screening test in stable adult patients with blunt abdominal trauma: a Greek study. European Radiology, 20(1), pp.234–238.
- Melniker LA, Leibner E, McKenney MG, Lopez P, Briggs WM, Mancuso CA. Randomized controlled clinical trial of point-of-care, limited ultrasonography for trauma in the emergency department: the first sonography outcomes assessment program trial. Ann Emerg Med. 2006 Sep;48(3):227-35. doi: 10.1016/j.annemergmed.2006.01.008
- Teixeira PG, Inaba K, Hadjizacharia P, et al. Preventable or potentially preventable mortality at a mature trauma center. J Trauma. 2007 Dec;63(6):1338-46; discussion 1346-7. doi: 10.1097/TA.0b013e31815078ae.
- Ollerton, J.E., Sugrue, M., Balogh, Z., D’Amours S.K., Giles, A., Wyllie, P. (2016). Prospective study to evaluate the influence of FAST on trauma patient management. J Trauma, 60(4):785–91. doi:10.1097/01.ta.0000214583.21492.
- Richards, J.R. and McGahan, J.P. (2017). Focused Assessment with Sonography in Trauma (FAST) in 2017: What Radiologists Can Learn. Radiology, 283(1), pp.30–48.
- Mohammadi, A. and Ghasemi-rad, M. (2012). Evaluation of gastrointestinal injury in blunt abdominal trauma “FAST is not reliable”: the role of repeated ultrasonography. World Journal of Emergency Surgery, 7(1),p.2.
- Fleming S, Bird R, Ratnasingham K, Sarker SJ, Walsh M, Patel B. Accuracy of FAST scan in blunt abdominal trauma in a major London trauma centre. Int J Surg. 2012;10(9):470-4. doi: 10.1016/j.ijsu.2012.05.011.
- Aboobakar, M.R., Singh, J.P., Maharaj, K., Mewa Kinoo, S. and Singh, B. (2017). Gastric perforation following blunt abdominal trauma. Trauma Case Reports,10, pp.12
- Chiu WC, Cushing BM, Rodriguez A, et al. Abdominal injuries without hemoperitoneum:a potential limitation of focused abdominal sonography for trauma (FAST). J Trauma 1997;42(4):617e23. discussion 623e5.
- McGahan JP, Richards JR. Blunt abdominal trauma:the role of emergant sonography and a review of the literature. AJR Am J Roentgenol 1999;172(4):897e903.
- McKenney KL, McKenney MG, Cohn SM, et al. Hemoperitoneum score helps determine need for therapeutic laperotomy. J.Trauma 2001;50(4):650e4. discussion 654e6.
- Farahmand N, Sirlin CB, Brown MA, et al. Hypotensive patients with blunt abdominal trauma: a performance of screening US. Radiology 2005;235(2):436e43.
- Lee BC, Ormsby EL, McGahan JP, Melendres GM, Richards JR. The utility of sonography for the triage of blunt abdominal trauma patients to exploratory laparotomy. AJR Am J Roentgenol 2007;188(2):415e21.
- Rothlin MA, Näf R, Amgwerd M, Candinas D, Frick T, Trentz O. Ultrasound in blunt abdominal trauma and thoracic trauma. J Trauma 1993;34(4):488e95.
- Wherrett LT, Boulanger BR, McLellan BA, et al. Hypotension after blunt abdominal trauma: the role of emergent abdominal sonography in surgical triage. J Trauma 1996;41(5):815e20.
- Bennett MK, Jehle D. Ultrasound in blunt abdominal trauma. Emerg Med ClinNorth Am 1997;15(4):763e87.