UDK: 618.6-083.98
Demjanski V1
1University Clinic for Traumatology, Orthopedic Diseases, Anesthesia, Reanimation, Intensive Care and Emergency Centre, Skopje, Macedonia
Abstract
Most of the newborns adapt well to extra-uterine life, but some of them need stabilization or resuscitation. Expressed as a percentage, 85% breathe on their own, 10% after stimulation, and about 5% require positive pressure ventilation. The incidence of intubations varies between 0.4% and 2%, about 0.3% require cardiac compressions, and only 0.05% receive adrenaline. There are known risk factors, antepartum and intrapartum, which are the most common reasons for forced stabilization or resuscitation.
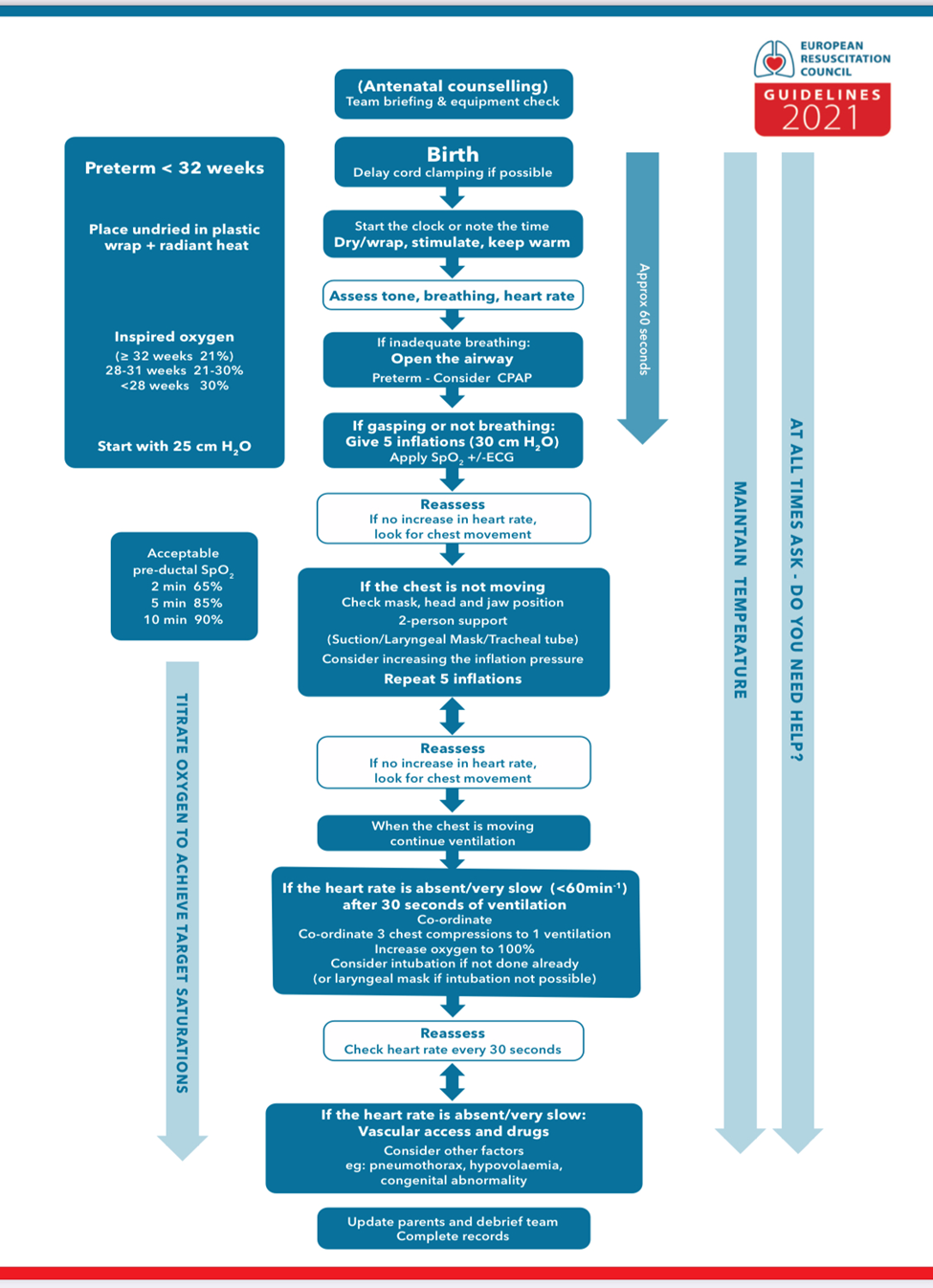
The protocols (European Resuscitation Council) have precise recommendations for each segment of resuscitation, starting with standards for personnel, equipment, environment; handling of the umbilical cord after birth; initial examination and assessment (tone, breathing, heart rate); and life support. The protocols have details that differ between full-term and premature newborns.
Resuscitation in the narrower sense of the word implies undertaking one or more of the four basic procedures (ABCD):
- Initial stabilization steps (warming, airway aspiration if necessary, drying, stimulation),
- Ventilation,
III. Heart compressions,
- Administer epinephrine and/or volume replacement.
It is of crucial importance to respect the “Golden Minute” rule, i.e., taking initial measures, re-evaluation and starting ventilation, if necessary, within 60 seconds.
After recovery of vital signs and adequate ventilation and circulation, the newborn should be transferred to an intensive care unit under appropriate monitoring and care. Induced therapeutic hypothermia should be an option following a properly prescribed implementation protocol. Failure to establish ROSC in neonates after 10-20 minutes of intensive resuscitation is associated with a high risk of mortality and a high risk of neurological damage in survivors. Refraining from applying resuscitation measures is reasonable in cases with a certain poor prognosis (gestational week <22 weeks and/or bw<350g; anencephaly; major chromosomal abnormalities), a decision for which with prior consultation and discussion with the parents is preferred.
Key words: newborn resuscitation, newborn life-support, resuscitation guidelines.
Introduction
Newborn resuscitation is a critical medical procedure aimed at reviving newborns who experience breathing difficulties or have trouble adapting to life outside the womb. As medical professionals, it is crucial to stay informed about the latest guidelines and the best practices in newborn resuscitation to ensure the best possible outcomes for these vulnerable patients. In this article, we will present the fundamental principles and techniques of newborn resuscitation while emphasizing the importance of continuous education and adherence to current guidelines. They apply primarily to newly born infants undergoing transition from intrauterine to extrauterine life, but the recommendations are also applicable to neonates who have completed perinatal transition and require resuscitation during the first few weeks to months following birth.
The European Resuscitation Council (ERC) Guidelines provide a comprehensive framework for healthcare providers to manage newborn resuscitation and support the transition of infants at birth.
Newborn Resuscitation and Support of Transition of Infants at Birth
Up to 85% of the newborns breathe spontaneously without intervention; a further 10% respond after drying, stimulation and airway opening maneuvers; approximately 5% receive positive pressure ventilation. Intubation rates vary between 0.4% and 2%. Fewer than 0.3% of the infants receive chest compressions and only 0.05% receive adrenaline.
Number of risk factors has been identified as increasing the likelihood of requiring help with stabilization, or resuscitation. Antepartum risk factors could be fetal (intrauterine growth restriction, <37 weeks gestation, serious congenital abnormality) and maternal (infections, gestational diabetes, pregnancy-induced hypertension, pre-eclampsia, high BMI, short stature). Intrapartum factors include evidence of fetal compromise (non-reassuring CTG etc.), meconium- stained amniotic fluid, forceps or vacuum delivery, significant bleeding, emergency C-section, general anesthesia.
Developing a comprehensive algorithm for newborn’s life support is essential to guide healthcare professionals in providing immediate and effective care to infants in distress. This algorithm provides a step-by-step guide for healthcare professionals in providing life support for newborns. It covers assessment, initial steps and advanced interventions in accordance with the European Resuscitation Council Guidelines.
Initial Assessment and Identification
Immediate Assessment
Place the newborn on a warm, dry surface. Ensure a clear airway by gently suctioning the mouth and nose if needed. Assess breathing, heart rate, muscle tone, reflex irritability and color using the Apgar score.
Thermal Control Recommendations
The newborn infant’s head and body should be immediately covered with a warm and dry towel to prevent further heat loss. Its body temperature should be monitored regularly after birth, in order to avoid hypothermia or hyperthermia and it should be maintained between 36.50C and 37.50C. In case resuscitation is required, the newborn should be placed on a warm surface. As far as premature babies are concerned, recommendations include increased room temperature, warm blankets, head cap and thermal mattress.
Classification according to Initial Assessment
Based on the initial assessment, the infant can usually be placed into one of three groups:
- Satisfactory transition (good tone, vigorous breathing or crying, heart rate>100min) – does not require support, only maintenance of the body temperature;
- Incomplete transition (reduced tone, breathing inadequately (or apneic), heart rate <100 min) – it requires maintaining the airway, lung inflation and ventilation, as well as
continuously assessment of the changes in heart rate and breathing;
- Poor/failed transition (floppy, pale, breathing inadequately or apneic, heart rate <60 min or undetectable) – the cord should be clamped immediately, continue with ventilation and asses the changes in heart rate and breathing.
Newborn Life Support
Airway
Ensuring an open airway, aerating and ventilating the lungs, is usually all that is necessary. For this purpose, the newborn should be placed on his back, with the head in a neutral position. In floppy infants, pulling the jaw forwards (jaw lift) may be essential in opening and/or maintaining the airway and reducing mask leak. If having difficulty providing both jaw lift and ventilation, an oropharyngeal on nasopharyngeal airway should be used. Attention should be paid to airway obstruction from meconium, mucus blood cloths or vernix and aspirate if necessary.
Breathing & circulation
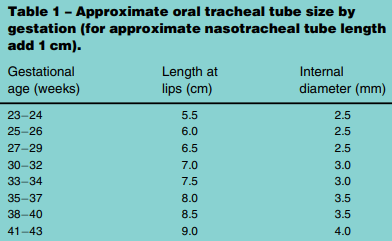
If the newborn is apneic, gasping or not breathing effectively, aim to start positive pressure ventilation as soon as possible – ideally within 60 seconds of birth. Give five “inflations” via face mask maintaining the inflation pressure for up to 2-3 seconds. Provide initial inflation pressures of 30cm H2O for term infants commencing with air. Start with 25cm H2O for preterm infants <32 weeks using 21-30% inspired oxygen (21% inspired oxygen for term infants). The heart rate should be checked (whether it increases or there is no response), as well as chest movements. If the heart rate rises and the chest rises, it means that ventilation is effective and, in that case, it should be continued with ventilation 30/min until the newborn starts to breathe adequately. If there is no response in terms of increased heart rate or adequate breathing, rechecking of the newborn’s position, as well as ventilation techniques and/or ensuring a safe airway with a laryngeal mask or endotracheal intubation should be undertaken.
For this purpose, it is recommended to use a video laryngoscope, and to check the position of the tube by all available methods (auscultation, etCO2 appearance, evidence of adequate ventilation through demonstrating adequate expired tidal volume (about 5-8mL/kg), visible evidence of chest rise or chest X-ray). Аs for the fraction of inspired oxygen, the following recommendations are given:
Term and late preterm infants 35 weeks – In infants receiving respiratory support at birth, begin with air (21%).
Preterm infants <35 weeks – Resuscitation should be initiated in air or a low inspired oxygen concentration based on gestational age:
- 32 weeks 21%,
- 28-31 weeks 21-30%,
- <28 weeks 30%.
In infants <32 weeks gestation the target should be to avoid an oxygen saturation below 80% and/or bradycardia at 5 minutes of age. Both are associated with poor outcome.
Regarding mechanical ventilation, CPAP (in preterm infants with spontaneous breathing) and use of PEEP of 5-6cmH2O are recommended. If even after 30 seconds of ventilation the heart rate is not adequate (<60/min or absent), chest compressions should be applied. It is recommended to use a synchronous technique, providing three compressions to one ventilation at about 15 cycles every 30 seconds and to use a two-handed technique for compressions if possible. The response should be re-evaluated every 30 seconds. If there is no response, vascular access and drugs should be considered. If peripheral venous access cannot be established, umbilical venous access or intraosseous can be used. Central venous access is sometimes required.
Drugs
Although medications are rarely needed, they should be considered when there is no adequate response to ventilation and chest compressions. The recommendations are as follows:
- Adrenaline
- When effective ventilation and chest compressions have failed to increase the heart rate above 60/min;
- Intravenous or intraosseous is the preferred route – at a dose of 10-30micrograms/kg (0.1-0.3 mL/kg of 1:10,000 adrenaline [1000 micrograms in 10 mL]);
- Intra-tracheally if intubated and no other access available – at a dose of 50-100micrograms/kg;
- Subsequent doses every 3-5minutes if heart rate remains< 60/min.
- Glucose
- In a prolonged resuscitation to reduce likelihood of hypoglycemia;
- Intravenous or intraosseous: 250mg/kg bolus (2.5mL/kg of 10% glucose solution).
- Volume replacement
- With suspected blood loss or shock unresponsive to other resuscitative measures;
- Intravenous or intraosseous: 10mL/kg of group O Rh-negative blood or isotonic crystalloid.
- Sodium bicarbonate
- May be considered in a prolonged unresponsive resuscitation with adequate ventilation to reverse intracardiac acidosis;
- Intravenous or intraosseous: 1-2mmol/kg sodium bicarbonate (2-4 mL/kg of 4.2% solution) by slow intravenous injection.
- Naloxone – In situations of persistent apnea
- Intramuscular – an initial 200 microgram dose may help in thefew infants who, despite resuscitation, remain apneic with good cardiac output when the mother is known to have received opioids in labor. Effects may be transient, so continued monitoring of respiration is important.
Post-resuscitation Care
When the newborn infant responds positively to resuscitation, post-resuscitation care follows. It should be placed in an intensive care unit with continuous monitoring of vital parameters. Among other things, it is important to monitor closely the following parameters:
- Blood glucose level – in order to avoid hypo/hyperglycemia,
- Body temperature – consider inducing hypothermia to 33-340C in situations where there is clinical and/or biochemical evidence of significant risk of moderate or severe HIE (hypoxic-ischemic encephalopathy).
When to withold the resuscitation?
In situations where there is an extremely high mortality rate (>90%), resuscitation is not recommended, but it is always indicated in conditions associated with at least 50% survival rate. In conditions where there is low survival (<50%) and a high rate of morbidity, and where the anticipated burden of medical treatment for the child is high, parental wishes regarding resuscitation should be sought and usually supported.
When to discontinue the resuscitation?
If the heart rate of a newborn term infant remains undetectable for more than 20 minutes after birth despite the provision of all recommended steps of resuscitation and exclusion of reversible causes, consider stopping resuscitation.
Conclusion
Newborn resuscitation demands a systematic and evidence-based approach outlined in the latest guidelines to optimize outcomes. Healthcare providers must stay updated with these guidelines, employing proper assessment techniques, effective positive pressure ventilation and appropriate interventions. Mastery of the skills, techniques and decision-making processes involved in newborn resuscitation is crucial for medical professionals to ensure the best possible outcomes for neonates in distress. By adhering to and implementing these guidelines, medical professionals can provide effective and timely interventions during this critical transitional period, ultimately improving neonatal survival rates.
References:
- Ersdal HL, Mduma E, Svensen E, Perlman JM. Early initiation of basic resuscitation interventions including face mask ventilation may reduce birth asphyxia related mortality in low-income countries: a prospective descriptive observational study. Resuscitation 2012;83:86973.
- Perlman JM, Risser R. Cardiopulmonary resuscitation in the delivery room: associated clinical events. Arch PediatrAdolesc Med 1995;149:20-5.
- Barber CA, Wyckoff MH. Use and efficacy of endotracheal versus intravenous epinephrine during neonatal cardiopulmonary resuscitation in the delivery room. Pediatrics 2006;1189:102834.
- Halling C, Sparks JE, Christie L, Wyckoff MH. Efficacy of intravenous and endotracheal epinephrine during neonatal cardiopulmonary resuscitation in the delivery room. J Pediatr 2017;185:2326.
- Bjorland PA, Oymar K, Ersdal HL, Rettedal SI. Incidence of newborn resuscitative interventions at birth and short-term outcomes: a regional population-based study. BMJPaediatr Open 2019;3: e000592.
- Skare C, Boldingh AM, Kramer-Johansen J, et al. Video performance-debriefings and ventilation-refreshers improve quality of neonatal resuscitation. Resuscitation 2018;132:1406.
- Niles DE, Cines C, Insley E, et al. Incidence and characteristics of positive pressure ventilation delivered to newborns in a US tertiary academic hospital. Resuscitation 2017;115:1029.
- Wyckoff MH, Wyllie J, Aziz K, et al. Neonatal Life Support 2020 International Consensus on Cardiopulmonary Resuscitation and Emergency Cardiovascular Care Science With Treatment Recommendations. Resuscitation 2020;156:A15687,.
- Aziz K, Chadwick M, Baker M, Andrews W. Ante- and intra-partum factors that predict increased need for neonatal resuscitation. Resuscitation 2008;79:44452,.
- Annibale DJ, Hulsey TC, Wagner CL, Southgate WM. Comparative neonatal morbidity of abdominal and vaginal deliveries after uncomplicated pregnancies. Arch PediatrAdolesc Med 1995;149:8627.
- Liljestrom L, Wikstrom AK, Agren J, Jonsson M. Antepartum risk factors for moderate to severe neonatal hypoxic ischemic encephalopathy: a Swedish national cohort study. ActaObstetGynecolScand 2018;97:61523.
- Lee J, Lee JH. A clinical scoring system to predict the need for extensive resuscitation at birth in very low birth weight infants. BMC Pediatr 2019;19:197,.
- Londero AP, Rossetti E, Pittini C, Cagnacci A, Driul L. Maternal age and the risk of adverse pregnancy outcomes: a retrospective cohort study. BMC Pregnancy Childbirth 2019;19:261.
- Apgar V. A proposal for a new method of evaluation of the newborn infant. Curr Res AnesthAnalg 1953;32:2607 https://www.ncbi.nlm. nih.gov/pubmed/13083014.
- Trevisanuto D, Testoni D, de Almeida MFB. Maintaining normothermia: why and how? Semin Fetal Neonatal Med 2018;23:3339,
- Chua C, Schmolzer GM, Davis PG. Airway manoeuvres to achieve upper airway patency during mask ventilation in newborn infants – An historical perspective. Resuscitation 2012;83:4116.
- Bhalala US, Hemani M, Shah M, et al. Defining optimal head-tilt position of resuscitation in neonates and young infants using magnetic resonance imaging data. PLoS One 2016;11:e0151789.
- Wyllie J, Perlman JM, Kattwinkel J, et al. Part 7: Neonatal resuscitation: 2015 International Consensus on Cardiopulmonary Resuscitation and Emergency Cardiovascular Care Science with Treatment Recommendations. Resuscitation 2015;95:e169201.
- Holte K, Ersdal HL, Eilevstjonn J, et al. Predictors for expired CO2 in neonatal bag-mask ventilation at birth: observational study. BMJ Paediatr Open 2019;3:e000544,
- . Muscedere JG, Mullen JB, Gan K, Slutsky AS. Tidal ventilation at low airway pressures can augment lung injury. Am J RespirCrit Care Med 1994;149:132734,
- Naik AS, Kallapur SG, Bachurski CJ, et al. Effects of ventilation with different positive end-expiratory pressures on cytokine expression in the preterm lamb lung. Am J RespirCrit Care Med 2001;164:4948.
- Schwindt EM, Hoffmann F, Deindl P, Waldhoer TJ, Schwindt JC. Duration to establish an emergency vascular access and how to accelerate it: a simulation-based study performed in real-life neonatal resuscitation rooms. PediatrCrit Care Med 2018;19:46876.
- Isayama T, Mildenhall L, Schmolzer GM, et al. The route, dose, and interval of epinephrine for neonatal resuscitation: a systematic review. Pediatrics 2020;146.
- Matterberger C, Baik-Schneditz N, Schwaberger B, et al. Blood glucose and cerebral tissue oxygenation immediately after birth an observational study. J Pediatr 2018;200:1923.
- Wyllie J, Jos Bruinenberg J, Roehr CC, Rüdiger M, Trevisanuto D. B. U. European Resuscitation Council Guidelines for resuscitation 2015 section 7 resuscitation and support of transition of babies at birth. Resuscitation 2015;95:24862.
- Katheria AC, Brown MK, Hassan K, et al. Hemodynamic effects of sodium bicarbonate administration. J Perinatol 2017;37:51820.
- Moreland TA, Brice JE, Walker CH, Parija AC. Naloxone pharmacokinetics in the newborn. Br J ClinPharmacol 1980;9:609 12
- Basu SK, Kaiser JR, Guffey D, et al. Hypoglycaemia and hyperglycaemia are associated with unfavourable outcome in infants with hypoxic ischaemic encephalopathy: a post hoc analysis of the CoolCap Study. Arch Dis Child Fetal Neonatal Ed 2016;101:F14955,
- Perlman JM,Wyllie J, Kattwinkel J, et al. Neonatal resuscitation: 2010 International Consensus on Cardiopulmonary Resuscitation and Emergency Cardiovascular Care Science with Treatment Recommendations. Pediatrics 2010;126:e131944.
- Shah P, Anvekar A, McMichael J, Rao S. Outcomes of infants with Apgar score of zero at 10 min: the West Australian experience. Arch Dis Child Fetal Neonatal Ed 2015;100:F4924.
- Torke AM, Bledsoe P, Wocial LD, Bosslet GT, Helft PR. CEASE: a guide for clinicians on how to stop resuscitation efforts. Ann Am ThoracSoc 2015;12:4405, doi:http://dx.doi.org/10.1513/ AnnalsATS.201412-552PS.