Djordjevikj A1, Karadjova D1, Jovanovska V1, Dimitrioska R1, Kochovski G1, Mehmedovikj N2
1University Clinic for Gynecology and Obstetrics, Skopje
2University Clinic of State Cardiac Surgery
DOI: https://www.doi.org/10.55302/MJA237309dj
Abstract
Introduction: Numerous factors cause temperature imbalance in newborns during the adaptation period. Hypothermia in a newborn is defined as a body temperature below 36.5 ̊ C. It is classified as mild, moderate and severe. It is often represented in the early neonatal period and has an impact on morbidity in newborns. One of the causes of hypothermia is the first bath in the maternity ward. According to WHO recommendations, the first bath of newborns in the maternity hospital should be delayed for at least 24 hours. The aim of the study is the influence of the first bath on the BT of the newborn.
Material and Methods: Measurement of body temperature was performed with a digital thermometer. The study included term, healthy newborns. Hypothermic newborns were warmed under a radiation heater until thermostabilizing, bathed with running water, with a temperature of 35-37 ̊C, for no more than 5 minutes in a period of 4-6 hours after birth. BT was measured hourly, 20 minutes after bathing and hourly until thermostabilizing under a radiant heater.
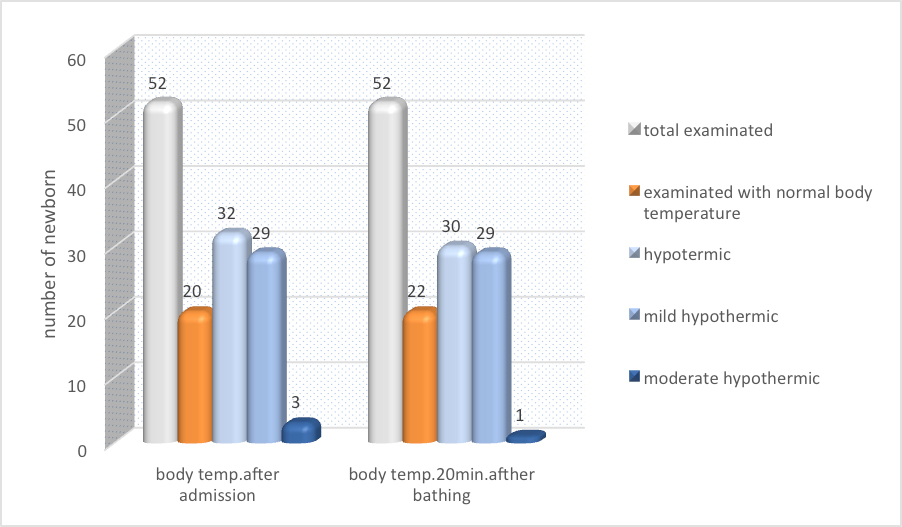
Results: In a study of 80 newborns examined, 52 met the criteria. Upon admission to the Basic Care Department, 61% of the examined newborns were hypothermic – 29 mildly hypothermic, 3 moderately hypothermic. 50% of newborns born with vaginal birth on admission to BCD were hypothermic, and 80% of those born by caesarean section. After 2 hours of admission to Basic Care Department, all neonates were thermostabilized except of 1 neonate (with borderline maturity). 20 minutes after bathing, 58% of newborns were hypothermic (29 mildly hypothermic, 1 with moderate hypothermia).
Conclusion: Thermal adaptation is faster in more mature newborns and in newborns born by vaginal delivery. Early first bath of term healthy newborns leads to mild hypothermia. Postponing of the first bath may be a good option to reduce hypothermia.
Key Words: body temperature, first bath, newborn
Introduction
Worldwide, 2.5 million children died in their first months of life, representing 47% of all deaths of children under five (1). The newborn, as the most vulnerable part of a population, has specific needs and is a sensitive marker for the quality of care. After birth, they begin with adaptation to breathing, adult type of circulation, as well as glucoregulation and thermoregulation – as part of metabolic adaptation.
Immediately after birth, in a transition period that lasts 6-10 hours, there are numerous factors that can interfere with the correct and smooth adjustment of body temperature (BT) and can lead to hypothermia. Neonatal hypothermia is a progressive decrease in the axillary temperature of the newborn (BT < 36.5°C), and it is categorized as mild hypothermia (36°C-36.4°C), moderate hypothermia (32°C-35.9°C) and severe hypothermia (<32°C) (2). Immediately after birth, 0.3̊ C/ min. body temperature or 1-3̊ C/ 5 min is lost. With stool and urine, 3% of BT is lost, transepidermal – with evaporation 27% and 70% with convection, conduction and radiation. In optimal environmental conditions, loss of BT is 35W/m² maximum loss of temperature, of which the newborn can compensate 70W/m².
Although hypothermia is rarely a direct cause of death, it contributes to a significant proportion of neonatal mortality globally, mostly as a comorbidity (3). The temperature should be maintained between 36.5°C and 37.5°C (1,2).
One of the factors for hypothermia is the first bath in the maternity ward. Bathing can be a stressful procedure for an infant, and it is shown that early first bathing destabilizes vitals in healthy neonates, particularly temperature, glucose levels, and respiratory status (4,5). In many hospitals, the first bath is done immediately after birth. It means that the neonate is separated from the mother, skin to skin contact is either lost or reduced and the breastfeeding is postponed (6).
According to WHO recommendations, it should be postponed 24 hours after birth or if it cannot be realized during this period, for cultural reasons, after 6 hours from birth at the earliest.
There are no strict recommendations for the timing of the first bath in healthy neonates. The objective of this study was to determine the impact of a first early bath on thermal adaptation and hypothermia in term healthy newborns.
Material and Methods
This is a prospective study performed at the University Clinic for Gynecology and Obstetrics, at the Department of Basic Care (DBC) of the newborn in a period of 4 weeks.
The study included all late-term neonates (37̊′⁷-41⁶′⁷gestational week) in the period between 01.02.2023 till 01.03.2023. Inclusion criteria for the study were late term neonates, healthy neonates. Exclusion criteria were all preterm infants, newborns that receive antibiotics, newborns transferred to neonatal ICU.
We evaluated mode of delivery (vaginal delivery or cesarean section), complications during labor and delivery, gestational age of the newborn, birth weight (BW), Apgar score, need for resuscitation and BT in different time points after birth. All newborns whose mother had complications during labor and delivery, as well as neonates that needed resuscitation were excluded from the study.
Ambient temperature in the DBC is 25̊ C. At the reception of the Department, admission of the newborn is carried out under a radiant heater (Drager, 400W – servo mode) and it consists in identification, measurement of BT and BW. The measurement of BT is carried out with a digital thermometer in a period of 5 minutes.
Newborn BT was monitored, depending on their condition on admission in DBC. Hypothermic newborns were warmed under a radiant heater until thermostabilizing, after which they were bathed with running water, with a temperature of 35-37 ̊C, for no longer than 5 minutes. Newborns with normal BT upon admission were bathed in a time interval of 4-6 hours after birth. This is followed by care of the newborn, with drying in warm clean diapers, care of the umbilicus, urogenital region, immunization and antihemorrhagic prophylaxis.
We measured BT on admission in DBC on every hour until bath, 20 minutes after bathing and until thermostabilizing under a radiant heater.
Results
80 newborns were examined, only 52 met the criteria and were included in the study. 8 newborns were in 37th gestational week (gw), 6 were 38th gw, 12 were 39th gw, 24 neonates were in 40th gw and 2 were in 41st gw. By type of birth, 32 were born with vaginal delivery, 20 with caesarean section.
On admission to DBC, 61% of the newborns were hypothermic – 29 were mildly hypothermic, 3 moderately hypothermic. 50% of those born with vaginal delivery were hypothermic and 80% of those born by caesarean section.
1 hour after admission to the DBC, 22 newborns were thermostabilized, 10 were still mildly hypothermic.
2 hours after admission to the DBC, all newborns were thermostabilized, except 1 newborn (with borderline maturity).
3 hours after admission to the DBC, all newborns were thermostabilized.
20 min after bathing 58% of the newborns were hypothermic – mildly hypothermic 29, 1 with moderate hypothermia. Newborns with normal BT at admission had 50% drop in temperature (1-2 ̊C) after bathing, while newborns that were hypothermic on admission to the DBC had 80% drop in BT (2-3 ̊C) after bathing.
6 hours after admission to the DBC, and 2 hours after the first bath all newborns were thermostabilized.
Table 1. Hypothermia in early first bath of newborns
Discussion
In a big systematic review by Priyadarshi and al from 2022, that included 16 studies and 39,020 healthy term newborns, regarding the time period of the first bath and thermal adaptation, they came to the conclusion that bathing the newborn within 24 hours of birth may reduce the risk of neonatal mortality and neonatal hypothermia compared to bathing in the first 24 hours, although these conclusions are limited by low-certainty evidence (7).
Bayih et al in their study in 2019, that included 403 newborns in Eastern Ethiopia, indicate a high prevalence of neonatal hypothermia in the adaptation period as a result of the absence of skin-to-skin contact with the mother, use of a cap, warm transport intra department and prematurity (8).
Kelly et al in their study in 2018, after monitoring BT of healthy term newborns with the first bath 3, 6, 9 hours after birth, indicate an insignificant difference in BT and normothermia after 2 hours of bathing in all three groups (9).
Compared to the large studies showing effects of early bathing versus delayed bathing on mortality of newborns, thermoregulation, glycemia, BW, breastfeeding, the aim of our study was to show the effect of early bathing on BT in the newborns in our maternity hospital and to compare the obtained results. This is a small segment of the temperature chain in which there is always room for correction and improvement.
Given that it is a small number of respondents, in a time interval of 4 weeks, the percentage value of the obtained results for hypothermia of newborns after bathing, in our study is higher. Differences are detected in the acceptance of the term delayed bathing. From a review of the literature and published results, in some maternity hospitals, delayed bathing is accepted 9 hours after the birth, in some 12 hours after birth, in others 24 hours after (10-12). Given the dynamics of work, the first bath of the newborn in our maternity hospital is 4-6 hours after birth, but in accordance to the adaptation and stability of vital parameters and BT of the newborn. Thermal adaptation is shorter in more mature newborns, than in newborns with borderline maturity. Newborns born with vaginal delivery have better thermal adaptation, compared to the newborns born with sectio ceasarea. In our study, we detect hypothermia of a mild degree after early bathing, which coincides with the published results of other authors (9). If, on admission to the DBC, newborns have a normal BT, after taking a bath, there is a smaller drop in BT, compared to the newborns who are hypothermic on admission to the department.
According to all available evidences, it is desirable to postpone the first bath 24 hours after birth. It is necessary to introduce a protocol for the first bath of a newborn in every maternity hospital, as well as to provide constant monitoring for its implementation, in accordance to the efforts to reduce the neonatal morbidity and improve the quality of work.
Conclusion
Thermal adaptation is faster in more mature newborns and in newborns born with vaginal delivery. Early first bath of term healthy newborns leads to mild hypothermia. Postponing of the first bath can be a good option to reduce hypothermia. A protocol for the first bath of a newborn and its implementation is needed in the efforts of reducing the neonatal morbidity and improving the quality of work.
References:
- WHO. Newborns: reducing mortality. 2019, https://www.who.int/news-room/fact-sheets/detail/newborns-reducing-mortality.
- WHO. Mother-baby package (WHO/RHT/MSM/97.2, Rev 1) Geneva: World Health Organization; 1997.
- Lunze K., Bloom D. E., Jamison D. T., Hamer D. H. The global burden of neonatal hypothermia: systematic review of a major challenge for newborn survival. BMC Medicine. 2013;11(1):24.
- Ruschel LM, Pedrini DB, and da Cunha MLC. Hypothermia and the newborn’s bath in the first hours of life. Rev Gaúcha Enferm. 2018; 39:e20170263.
- McInerney MC and Gupta A. Delaying the first bath decreases the incidence of neonatal hypoglycemia. J Obstet Gynecol Neonatal Nurs. 2015; 44:S73-4.
- Moore ER, Bergman N, Anderson GC, and Medley N. Early skin-to-skin contact for mothers and their healthy newborn infants. Cochrane Database Syst Rev. 2016;11:CD003519.
- Priyadarshki M, Baladionder B, Gupta S, Sankar MJ. Timing of first bath in term healthy newborns. A systematic review. Journal of Global health. 2022.
- Bayih W, Assefa N, Dheresa M, Minuye B, Demis S. Neonatal hypothermia and associated factors within six hours of delivery in eastern part of Ethiopia: a cross-sectional study. BMC Pediatrics 2019;19: 252.
- Kelly PA, Classen KA, Crandall CG, Crenshaw JT, Schaefer SA, and Wade DA. Effect of Timing of the First Bath on a Healthy Newborn’s Temperature. J Obstet Gynecol Neonatal Nurs. 2018; 47:608-19.
- Turney J, Lowther A, Pyka J, Mollon D, and Fields W. Delayed Newborn First Bath and Exclusive Breastfeeding Rates. Nurs Womens Health. 2019; 23:31-7.
- Long K, Rondinelli J, Yim A, Cariou C, and Valdez R. Delaying the First Newborn Bath and Exclusive Breastfeeding MCN Am J Matern Child Nurs. 2020; 45:110-5.
- Anderson J. An Organization-Wide Initiative to Implement Parent-Performed, Delayed Immersion Bathing. Nurs Womens Health. 2021; 25:63-70.