UDK: 616-089.5-032:611.14
Lleshi A.1, Brzanov-Gavrilovska A.1, Angjushev D.1, Ognjanova V.1, Trposka A.1, Mladenovska Cvetkova M.1
1 University Clinic for Traumatology, Orthopedic Diseases, Anesthesiology, Reanimation and Intensive Care Medicine and Emergency Department, Clinical Center “Mother Theresa” Faculty of Medicine, “Ss. Cyril and Methodius” University, Skopje, Republic of North Macedonia
Abstract
Introduction: Total Intravenous Anesthesia using Target Controlled Infusion is a sophisticated anesthesia technique that offers several advantages over traditional methods.
Material and Methods: In this pilot study, we randomly assigned 40 patients to two groups, each of which received different general anesthesia techniques. Group 1 (TIVA-TCI) initiated the induction with 20mg of Lidocaine, administered Propofol at 4mcg/ml using Marsh’s model, continuously administered Remifentanil at 4ng/ml using the Minto model Target Controlled Infusion Perfusor to target plasma concentration, administered Rocuronium bromide at 0.6mg/kg, and intubation after 90 seconds. We maintained anesthesia by continuously applying Propofol at dose of 2–6mcg/ml and remifentanil at dose of 2–6ng/ml using a Target-Controlled Infusion Perfusor, based on the Brain Electrical Activity Scale neuromonitoring value of BIS, the desired mean arterial pressure and the heart rate. Group 2 (SIA) underwent anesthesia induction using Lidocaine 20mg, Propofol 1-2mg/kg, a continuous Remifentanil infusion ranging from 3-6ng/ml based on the Minto model, and 0.6mg/kg of Rocuronium bromide administered 90 seconds before intubation. Sevoflurane inhalation with a target minimum alveolar concentration of 0.7–1.0 was used for anesthesia maintenance.
Results: The sevoflurane group had increased heart rate, systolic, diastolic and mean arterial pressure, particularly during intubation and extubating. The duration of extubating was shortened in the TIVA group. Additionally, liver function was safer when TIVA was utilized. Patients in the sevoflurane group experienced postoperative nausea and vomiting at a greater rate.
Conclusion: Target Controlled Infusion – Total Intravenous Anesthesia is considered superior in promoting a smoother and more comfortable patients’ perioperative experience.
Key Words: Breast surgery; Heart rate; Mean arterial pressure; Sevoflurane inhalational anesthesia; Total intravenous anesthesia-target controlled infusion; Postoperative nausea and vomiting.
Introduction
Breast cancer is the most common reason for breast surgery, while other reasons include the removal of a benign tumor, abscess drainage and cosmetic procedures. Once the cancer has been removed, the breast reconstruction might happen right during the original surgery or later. Anesthesia options include total intravenous anesthesia (TIVA) or a mix of inhaled and intravenous (IV) medicines (1). Total intravenous anesthesia (TIVA) in combination with Remifentanil and Propofol (RP) is the most efficient type of general anesthesia (GA) for patients undergoing medical procedures, both adult and pediatric (2). Increased safety and predictable timing have resulted from the introduction of commercially accessible pumps that use target-controlled infusion (TCI) approaches to better manage plasma concentration levels (2). A microprocessor is embedded in a TCI pump and is programmed with pharmacokinetic models for appropriate medications. The anesthesiologist chooses the medication and pharmacokinetic model that the TCI pump will use, as well as the patient’s information including body weight and age, and the target plasma or ‘brain’ (effect-site) concentration, with the pump deciding the first bolus and continuous administration rates (3). When paired with Propofol in target-controlled infusion (TCI) regimes, Remifentanil is preferred over other opioids for anesthesia due to its special pharmacologic qualities, which include a rapid onset of action, accurate intra-operative control, and a shortened recovery profile (2,4,5). The minimum alveolar concentration (MAC) is the gold benchmark for determining potency (7). The low blood: gas solubility of Sevoflurane enables prompt, seamless induction and recovery from anesthesia, as well as precise control of the stage of anesthesia (8). In order to improve drug administration and anesthesia level, the Brain Electrical Activity Scale (BIS) was developed by measuring the brain electrical activity of individuals who have been sedated (9). By lowering the likelihood of intraoperative awareness, the BIS represents a substantial advancement in the objective measurement of the level of anesthesia and gives anesthesia physicians useful real-time input. Range within 40-60 BIS is suitable for general anesthesia, either inhalational anesthesia or TIVA TCI (10). Additionally, there are growing numbers of severe health effects linked to climate change. When using inhalational anesthesia, the global warm potential of sevoflurane is lowest compared to other volatiles and it is 130. The global warming potential of propofol (TIVA) is around 1% that of sevoflurane volatile anesthesia (11).
The primary objective of this study was to compare the hemodynamic stability, time to induction and time to extubating between the two groups TIVA TCI and sevoflurane inhalational anesthesia (SIA). Additional objectives included comparing the two groups, TIVA TCI and SIA, with respect to the following measures: the Visual Analogue Scale (VAS) for postoperative pain after surgery; liver function as assessed by ALT, albumin, and AST; and postoperative nausea and vomiting (PONV).
Material and Methods
This prospective, randomized, interventional clinical study was carried out at University Clinic for Traumatology, Orthopedic disease, Anesthesiology, Reanimation and Intensive Care Medicine and Emergency Department and University Clinic for Plastic and Reconstructive Surgery, Skopje, involving patients undergoing breast reconstructive surgery after mastectomy due to breast cancer. We obtained approval from the Bioethics Committee of the Medical Faculty in Skopje. Every patient signed informed consent. For this pilot study we included 40 patients that were randomly assigned to two groups, each receiving different general anesthesia techniques. The first group were patients with total intravenous anesthesia-total controlled anesthesia (TIVA-TCI) and the second group were patients with sevoflurane inhalational anesthesia (SIA).
Inclusion criteria: Patients over 25 years to 75 years, with a signed written consent, BMI<35 kg/m2, American society of Anesthesiologist classification (ASA) I-II.
Exclusion criteria included patients younger than 25 years or older than 75 years, any past medical history of liver disease or preexisting liver dysfunction, renal insufficiency, cardiovascular or neurological disease, Diabetes mellitus, allergic diathesis, Body mass index (BMI) >35, patients using sedative and opioids, patients who had not signed written consent.
Group 1 (TIVA-TCI) initiated the induction with 40mg of Lidocaine, administered Propofol at 4 mcg/ml using Marsh’s model, continuously administered Remifentanil at 4ng/ml using the Minto model TCI Perfusor to target plasma concentration, administered Rocuronium bromide at 0.6mg/kg, and attempted intubation after 90 seconds. We maintained anesthesia by continuously applying propofol at a dose of 2–6mcg/ml and remifentanil at a dose of 2–6ng/ml using a TCI Perfusor, based on the BIS neuromonitoring value, the desired mean arterial pressure and the heart rate. Group 2 (SIA) underwent anesthesia induction using Lidocaine 20mg, Propofol 1-2mg/kg, a continuous Remifentanil infusion ranging from 3-6ng/ml based on the Minto model, and 0.6mg/kg of Rocuronium bromide administered 90 seconds before intubation. Sevoflurane inhalation with a MAC of 0.7–1.0 was used for anesthesia maintenance.
Mechanical ventilation, using the MV model-pressure control volume guarantee (PCV/VG) with a mixture of oxygen 50% and air 50%, was then administered. The flow rate was 2L/min, and the tidal volume (TV) was 6-8ml/kg. The respiratory rate was between 10-14 breaths per minute to maintain end tidal CO2 range of 35-45mmHg, and BIS values were between 40-60. Extubating occurred upon patients’ responsiveness to verbal commands and tracheal and laryngeal reflexes were restored. After extubating, all patients received 50mcg of Fentanyl. We monitored all patients intraoperatively for non-invasive blood pressure, heart frequency and mean arterial pressure.
We collected blood samples for extended laboratory testing in both study groups at four different time points: T1 (after induction of anesthesia in the operating room), T2 (after extubating in the recovery room-PACU) and T3 (24 hours after the end of the surgery).
We compared the induction time, which is the time from the onset of anesthesia to the disappearance of the eyelash response, the time to extubating, which is the time from the termination of anesthesia to the extubating, blood pressure, heart frequency, liver function, as measured by the values of alanine aminotransferase and aspartate aminotransferase, albumin, postoperative pain as measured by the Visual Analogue Scale (VAS), and postoperative nausea and vomiting.
Results
The statistical analyses were performed using SPSS version 26. The significance threshold for all statistical analyses was set at p<0.05. To compare the data, a student’s T test was employed.
The sample size was 40 subjects. Both groups were comparable in demographic data. Both groups had a similar average age. All patients in both groups were women. BMI was consistent between the two groups. ASA classifications were also consistent (Table 1).
Table 1. Patients demographics.
| Age | Age | Gender | BMI kg/m2 | BMI kg/m2 | ASA | |
| count | mean | count | count | mean | count | |
| Group | ||||||
| 1.0 | 20.0 | 45.2 | 0.0 | 20.0 | 23.0 | 0.0 |
| 2.0 | 20.0 | 46.6 | 0.0 | 20.0 | 23.49 | 0.0 |
BMI-Body mass index (kg/m2); ASA-American society of anesthesiologist classification
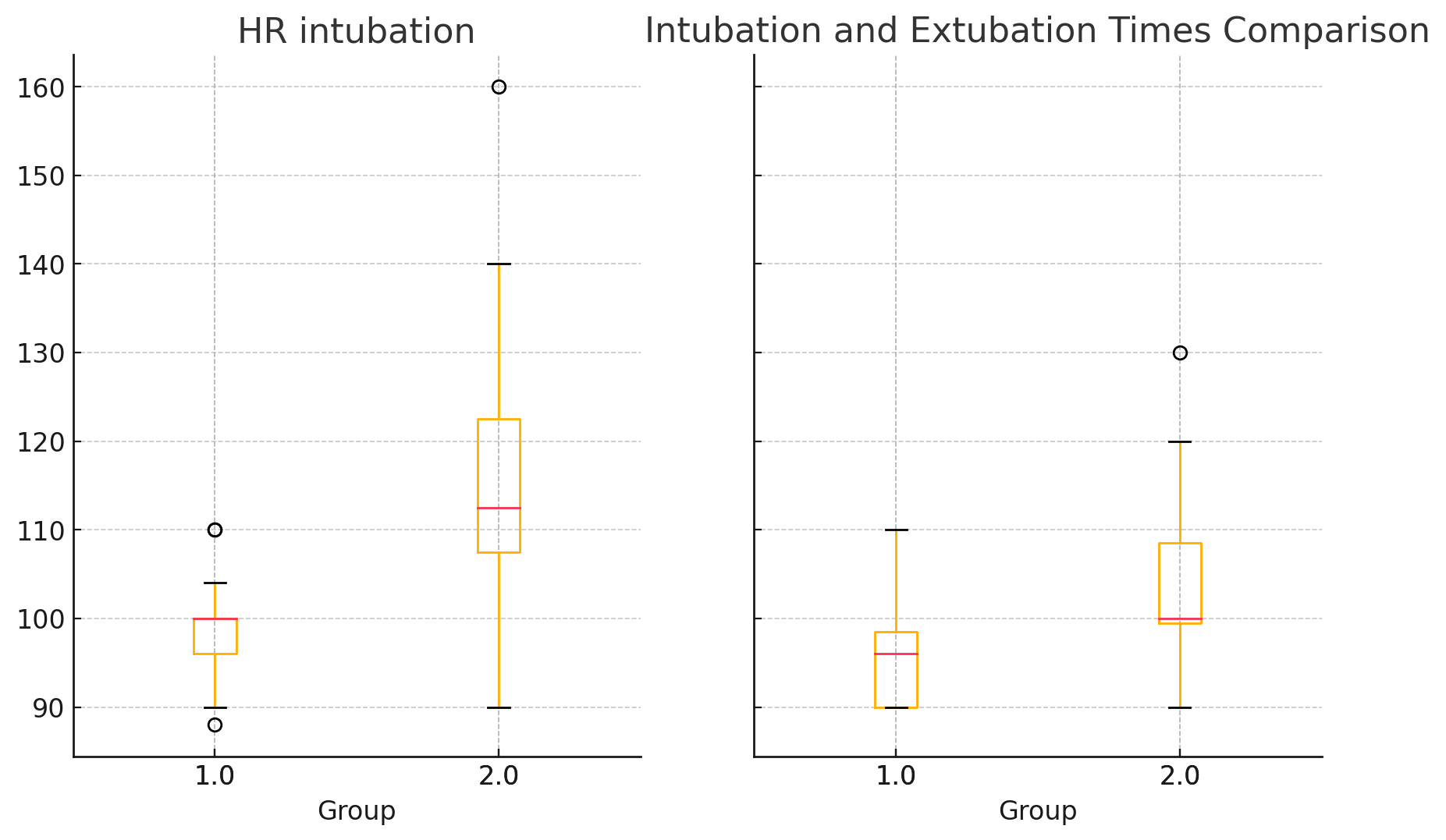
Heart rate and arterial tension, including mean arterial pressure (MAP) readings showed significant variations between the groups. Significant differences were observed in HR during intubation (p <0.05), intraoperative (p <0.05), extubating (p <0.05) and after extubating (p <0.05). Group 2 (SIA) had higher HR values compared to Group 1 (TIVA-TCI) (Table 2) (Figure 1).
Table 2. Comparison of hemodynamic data between two groups-heart rates in beats per minute.
| Heart rate – beats per minute | ||||||||||
| Intubation | Extubating | |||||||||
| Count | Mean | Min | 50% | Max | Count | Mean | Min | 50 % | Max | |
| Group | ||||||||||
| TIVA-TCI | 20.0 | 98.8 | 88.0 | 100.0 | 110.0 | 20.0 | 95.5 | 90.0 | 96.0 | 110.0 |
| SIA | 20.0 | 115.5 | 90.0 | 112.5 | 160.0 | 20.0 | 102.75 | 90.0 | 100.0 | 130.0 |
TIVA-TCI Total intravenous anesthesia-target controlled infusion group
SIA Sevoflurane inhalational group
Figure 1. Heart rate comparison at intubation and extubating point expressed in beats per minute.
Significant differences during intubation were noted in systolic blood pressure (p<0.05), with Group 2 (SIA) having higher values. Student’s T test; p<0.05 shows significant difference between groups; The analysis of the recorded values for diastolic blood pressure showed significant differences during intubation (p=0.002239) and extubating (p=0.042853), with Group 2 (SIA) showing higher values. MAP was also higher in the SIA group with statistically significant differences before intubation and after extubating p<0.05.
Average time to intubation in the TIVA group was 3.2 minutes and in the SIA group 3.9 minutes. Average time to extubating in the TIVA TCI group was 7.9 minutes and in the SIA group was 9.8 minutes respectively.
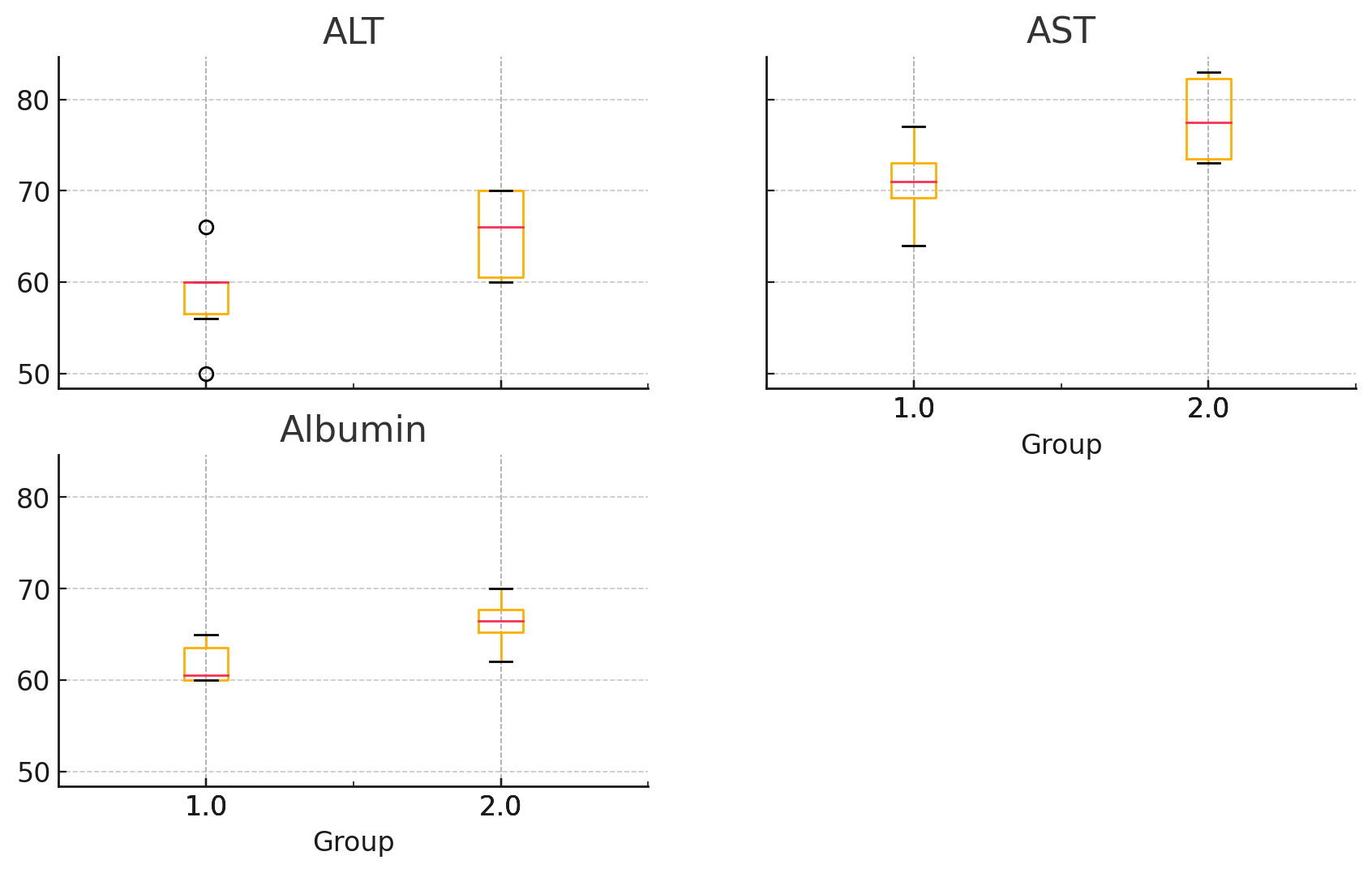
Regarding the liver function, Group 2 (SIA) had significantly higher ALT levels (p=0.024107) and higher AST levels (p=0.013136) as well as higher albumin levels (Figure 2).
Figure 2. Comparison of liver function between TIVA TCI and SIA group through ALT (U/L), AST (U/L) and albumin (g/L).
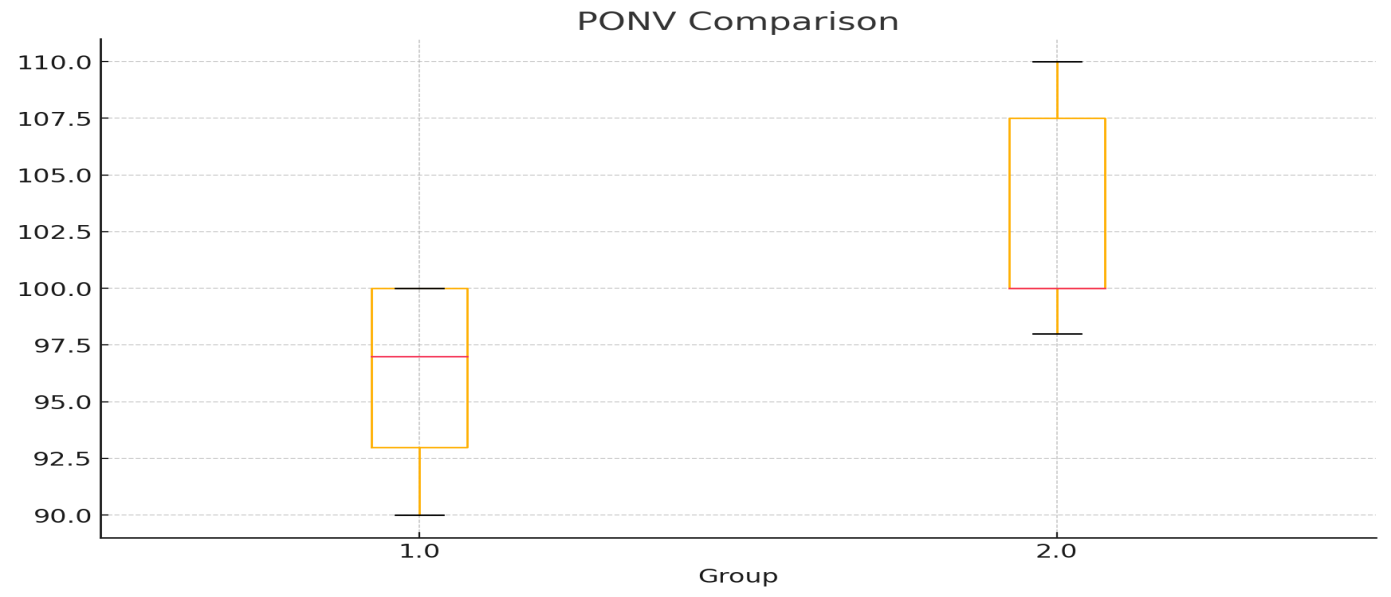
Group 2-SIA had significantly higher PONV scores (p=0.029095), indicating a higher incidence or severity of postoperative nausea and vomiting (Figure 3). 3 of our patients in TIVA group had a mild form of postoperative nausea and vomiting, and on the other side 7 of our patients in the sevoflurane group had postoperative nausea and vomiting. One of them had severe form and the other six – mild form. Every patient with PONV was given Metoclopramide 10mg intravenous.
Figure 3. Postoperative nausea and vomiting comparison between two groups-semi-quantitative percentage.
The VAS score for the TIVA-TCI group was significantly lower, with a mean score of 2.5 ± 1.7 compared to 3.9 ± 2.5 in the SIA group, representing a 35.9% reduction in pain levels, demonstrating significantly better pain management with the TIVA-TCI technique.
Only one patient had sore throat reported in the SIA group, while no complications were noted in the TIVA TCI group.
Discussion
In anesthesia, hemodynamic stability is among the most crucial factors. Although the two groups noted a comparable decrease in blood pressure, SIA group’s mean arterial pressure and heart rate increased much higher than the Propofol/ Remifentanil group ones. Same results were presented in the study of Juckenhöfel and coauthors (12). A comparable outcome was reported in the study of Shah et al., where sevoflurane group has notably higher heart rates after surgery at 5-, 10- and 15-minutes intervals, while the two groups did not show a significant variance in heart rates during intra-operative intervals, except at 45 and 60 minutes. Patients in Propofol group exhibited significantly low systolic and diastolic blood pressure from after insufflation until the surgery was finished (13). He Lu et al. in their study for spine surgery found out that the TIVA group exhibited lower changes in heart frequency and mean arterial pressure compared to the desflurane group. Furthermore, in the time of extubating, the heart rate and MAP were lower in the TIVA group (14). Our findings suggest that Sevoflurane inhalational group experienced more hemodynamic instability with higher heart rates and higher systolic and diastolic blood pressure especially in the time of intubation and extubating, which is consistent with previous findings. Another concern that anesthesiologists are particularly interested in is extubating time since it might be impacted by various anesthetic medications or procedures. Hence, for the purpose to increase OR efficiency, anesthesiologists must select the right anesthetic medications or procedures to prevent extended extubating. The main conclusions of Lai H et al. retrospective study demonstrate that in comparison to inhalational anesthesia with desflurane, propofol-based TIVA TCI shortened the extubating duration. The TIVA group’s 0.9-minute extubating time decrease showed less of a clinical or financial impact on the anesthetic controlled time component of operating time efficiency, even if statistically significant discrepancies were found. Furthermore, they discovered that in patients having open major upper abdomen surgery, the following characteristics are associated with extended extubating: age, gender, BMI and length of anesthesia (1). Our patients were comparable in age, gender, BMI and length of anesthesia. According to our results patients in the TIVA TCI group experienced faster extubating time compared to the SIA group as in the study of Lai H. On the other side, the average recovery and extubating times in the two groups were comparable, according to the findings of Magni’s investigation and study of Yang L et coauthors. (15,16). According to surveys, even more so than pain, PONV is the most feared anesthetic side effect. Every episode of PONV causes a 20-minutes delay in postoperative care unit discharge, and 1% of patients undergoing day surgery are hospitalized as a result (17). Pharmacological therapies following anesthesia may be the breaking point for minimizing the frequency of PONV. Volatile anesthetics can increase the incidence of PONV, while TIVA can decrease it claims Yang Li in his study (16). Females, non-smoking status, people younger than 50 years, as well as use of inhalational anesthetics and anesthesia lasting longer than an hour are related to higher risk of PONV (17,18). The main cause of PONV in the very initial postoperative phase has been identified as the quantity of volatile anesthetic exposure. Moreover, postoperative nausea and vomiting have been related to opioids because of the sensitivity of the chemoreceptor trigger zone in area postrema to them (18). Uncertainty surrounds its exact mode of action however it seems to boost the function of gamma-aminobutyric acid (GABA) receptors, which in turn blocks synaptic transmission in the brain’s vomiting center—a group of medulla structures close to the fourth ventricle (19). Johnson K. in his study claims that Because of its benefits, TIVA is an anesthetic method chosen for patients who have experienced postoperative nausea and vomiting in the past or who are at a high risk of experiencing it. On the other side, this approach has some drawbacks and hazards, such as a modest increase in consciousness, an unintended hypotension linked to propofol distribution, and a risk of hyperalgesia with TIVA procedures that use high dose opioids (20). Our study highlights the use of total intravenous anesthesia. Liver function can be checked through Albumin, alanine aminotransferase (ALT) and aspartate aminotransferase (AST). Kim et al. in their study compared the liver and renal function in patients with thyroidectomy and reported that postoperative liver impairment was clinically inconsequential between the two groups. They showed that although postoperative AST readings in the sevoflurane group were higher than in TIVA group, they were still within the referent range. There were no variations in ALT between the two groups relative to the beginning (21). Sahin et al. supported these results in their publication for volatile anesthetics and TIVA in patients with lumbar discectomy and showed no clinical significance in the liver function between the two groups (22). We reported opposite results in our study since the patients in the sevoflurane group in our pilot trial had increased baseline ALT and AST levels, out of the normal range, indicate a higher level of hepatic impairment. VAS score showed significant difference in pain management between the two groups in our study, with reduction in pain levels in the TIVA TCI group. Comparable results have been published in the study of Tan T et al., Meng W. on the second postoperative day, and in the study of Hofer C. and coauthors where in the group receiving sevoflurane anesthesia, the amount of opioids used to produce a comparable level of postoperative pain was substantially higher (23,24,25).
Conclusion
This study highlights the use of TIVA-TCI for better hemodynamic stability in patients undergoing breast reconstructive surgery. Furthermore, the TCI-TIVA approach has a reduced incidence of PONV and produces better quality recovery in the early postoperative phase. TIVA is considered superior in promoting a smoother and more comfortable perioperative experience for patients.
References
- Lai HC, Lai MF, Huang YH, Yu JC, Tseng WC, Wu ZF. Comparison of Single Target-Controlled Infusion Pump-Delivered Mixed Propofol and Remifentanil with Two Target-Controlled Infusion Pumps-Delivered Propofol and Remifentanil in Patients Undergoing Breast Cancer Surgery-A Prospective Study. Int J Environ Res Public Health. 2023 Jan 23;20(3):2094. doi: 10.3390/ijerph20032094. PMID: 36767461; PMCID: PMC9915350.
- Deng X, Zhu T. Clinical comparison of propofol-remifentanil TCI with sevoflurane induction/maintenance anesthesia in laparoscopic cholecystectomy. Pak J Med Sci. 2014 Sep;30(5):1017-21. doi: 10.12669/pjms.305.5196. PMID: 25225518; PMCID: PMC4163224.
- Nimmo AF, Absalom AR, Bagshaw O, et al. Guidelines for the safe practice of total intravenous anaesthesia (TIVA): Joint Guidelines from the Association of Anaesthetists and the Society for Intravenous Anaesthesia. Anaesthesia. 2019 Feb;74(2):211-224. doi: 10.1111/anae.14428. Epub 2018 Oct 31. PMID: 30378102.
- Vuyk J. Pharmacokinetic and pharmacodynamic interactions between opioids and propofol. J Clin Anesth. 1997 Sep;9(6 Suppl):23S-26S. doi: 10.1016/s0952-8180(97)00117-7. PMID: 9278851.
- Santonocito C, Noto A, Crimi C, Sanfilippo F. Remifentanil-induced postoperative hyperalgesia: current perspectives on mechanisms and therapeutic strategies. Local Reg Anesth. 2018 Apr 9; 11:15-23. doi: 10.2147/LRA.S143618. PMID: 29670398; PMCID: PMC5898588.
- Miller AL, Theodore D, Widrich J. Inhalational Anesthetic. [Updated 2023 May 1]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK554540/.
- Aranake A, Mashour GA, Avidan MS. Minimum alveolar concentration: ongoing relevance and clinical utility. Anaesthesia. 2013 May;68(5):512-22. doi: 10.1111/anae.12168. Epub 2013 Feb 16. PMID: 23414556.
- Delgado-Herrera L, Ostroff RD, Rogers SA. Sevoflurance: approaching the ideal inhalational anesthetic. a pharmacologic, pharmacoeconomic, and clinical review. CNS Drug Rev. 2001 Spring;7(1):48-120. doi: 10.1111/j.1527-3458. 2001.tb00190.x. PMID: 11420572; PMCID: PMC6741648.
- Punjasawadwong Y, Phongchiewboon A, Bunchungmongkol N. Bispectral index for improving anaesthetic delivery and postoperative recovery. Cochrane Database Syst Rev. 2014 Jun 17;2014(6):CD003843. doi: 10.1002/14651858.CD003843.pub3. Update in: Cochrane Database Syst Rev. 2019 Sep 26;9:CD003843. doi: 10.1002/14651858.CD003843.pub4. PMID: 24937564; PMCID: PMC6483694.
- Mathur S, Patel J, Goldstein S, et al. Bispectral Index. [Updated 2023 Nov 6]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK539809/.
- McGain F, Muret J, Lawson C, Sherman JD. Environmental sustainability in anaesthesia and critical care. Br J Anaesth. 2020 Nov;125(5):680-692. doi: 10.1016/j.bja.2020.06.055. Epub 2020 Aug 12. PMID: 32798068; PMCID: PMC7421303.
- Juckenhöfel S, Feisel C, Schmitt HJ, Biedler A. TIVA mit Propofol/Remifentanil oder balancierte Anästhesie mit Sevofluran/Fentanyl bei laparoskopischen Operationen. Hämodynamik, Aufwachverhalten und Nebenwirkungen [TIVA with propofol-remifentanil or balanced anesthesia with sevoflurane-fentanyl in laparoscopic operations. Hemodynamics, awakening and adverse effects]. Anaesthesist. 1999 Nov;48(11):807-12. German. doi: 10.1007/s001010050789. PMID: 10631440.
- Shah J, Varma N. Comparison of hemodynamic stability and recovery profile with sevoflurane as inhalational agent versus propofol as total intravenous anesthesia during laparoscopic surgeries. Anaesth Pain & Intensive Care 2018;22(2)212-218.
- Lu, C.-H., Wu, Z.-F., Lin, B.-F., et al. Faster extubation time with more stable hemodynamics during extubation and shorter total surgical suite time after propofol-based total intravenous anesthesia compared with desflurane anesthesia in lengthy lumbar spine surgery. Journal of Neurosurgery: Spine, 2016; 24(2), 268–274. doi:10.3171/2015.4.spine141143.
- Magni G, Baisi F, La Rosa I, Imperiale C, Fabbrini V, Pennacchiotti ML, Rosa G. No difference in emergence time and early cognitive function between sevoflurane-fentanyl and propofol-remifentanil in patients undergoing craniotomy for supratentorial intracranial surgery. J Neurosurg Anesthesiol. 2005 Jul;17(3):134-8. doi: 10.1097/01.ana.0000167447.33969.16. PMID: 16037733.
- Yang L, Xu YJ, Shen J, Lou FF, Zhang J, Wu J. Propofol-based total intravenous anesthesia decreases the incidence of postoperative nausea and vomiting without affecting flap survival in free flap breast reconstruction. Gland Surg. 2020 Oct;9(5):1406-1414. doi: 10.21037/gs-20-225. PMID: 33224816; PMCID: PMC7667098.
- Iqbal, I. M., & Spencer, R. (2012). Postoperative nausea and vomiting. Anaesthesia & Intensive Care Medicine, 13(12), 613–616. doi: 10.1016/j.mpaic.2012.09.012
- Lingle, Chelsea L., “Prevention of Postoperative Nausea and Vomiting with Subhypnotic Doses of Propofol” (2019). Nursing Capstones. 191. https://commons.und.edu/nurs-capstones/191.
- Vuyk J , Sitsen E , Reekers M . Intravenous anesthetics . In: Miller RD , ed. Miller’s Anesthesia , 8th ed. Philadelphia : Elsevier/ Saunders ; 2015 : 821–63
- Johnson, K. Advantages, Disadvantages, and Risks of TIVA/TCI. 2017; 10.1007/978-3-319-47609-4_32.
- Kim JW, Kim JD, Yu SB, Ryu SJ. Comparison of hepatic and renal function between inhalation anesthesia with sevoflurane and remifentanil and total intravenous anesthesia with propofol and remifentanil for thyroidectomy. Korean J Anesthesiol. 2013 Feb;64(2):112-6. doi: 10.4097/kjae.2013.64.2.112. Epub 2013 Feb 15. PMID: 23459368; PMCID: PMC3581778.
- Sahin SH, Cinar SO, Paksoy I, Sut N, Oba S. Comparison between low flow sevoflurane anesthesia and total intravenous anesthesia during intermediate-duration surgery: effects on renal and hepatic toxicity. Hippokratia. 2011 Jan;15(1):69-74. PMID: 21607040; PMCID: PMC3093149.
- Tan, T., Bhinder, R., Carey, M., & Briggs, L. Day-Surgery Patients Anesthetized with Propofol Have Less Postoperative Pain than Those Anesthetized with Sevoflurane . Anesthesia & Analgesia,2010; 111(1), 83–85. doi:10.1213/ane.0b013e3181c0ee9e.
- Meng W, Yang C, Wei X, Wang S, Kang F, Huang X, Li J. Type of anesthesia and quality of recovery in male patients undergoing lumbar surgery: a randomized trial comparing propofol-remifentanil total i.v. anesthesia with sevoflurane anesthesia. BMC Anesthesiol. 2021 Dec 1;21(1):300. doi: 10.1186/s12871-021-01519-y. PMID: 34852781; PMCID: PMC8638110.
- Hofer, C. K., Zollinger, A., Bu¨chi, S., et al. Patient well-being after general anaesthesia: a prospective, randomized, controlled multi-centre trial comparing intravenous and inhalation anaesthesia. British Journal of Anaesthesia, 2003; 91(5), 631–637. doi:10.1093/bja/aeg243.