UDK: 616-005.4:616.75-089.87
Naumovski F1, Chavkoska M2, Ognjanova V1, Savevski A3, Gjorgjijeska K3, Nikolovski N3
1 University Clinic for Traumatology, Orthopedics, Anesthesiology, Resuscitation, Intensive Care and Emergency Center – Skopje, Department of Anesthesiology, Resuscitation and Intensive Care Medicine, “Ss. Cyril and Methodius” University Skopje, Faculty of Medicine
2 General Hospital Ohrid – Department of Anesthesiology and Intensive Care Medicine
3 University Clinic for Traumatology, Orthopedics, Anesthesiology, Resuscitation, Intensive Care and Emergency Center – Skopje, Department of Orthopedics, “Ss. Cyril and Methodius” University – Skopje, Faculty of Medicine
Abstract
Compartment syndrome is an agonizing state arising from excessive pressure buildup within muscles, hindering blood circulation and depriving nerve and muscle cells of vital oxygen and nutrients. Usually, this condition arises following injury-induced bleeding or swelling. The elevated pressure characteristic of compartment syndrome impedes the circulation of blood, oxygen and essential nutrients to and from the impacted tissues. In some cases, it necessitates immediate surgical intervention to avert lasting damage. Consensus holds that prompt intervention offers the greatest opportunity for full recovery and for averting additional tissue necrosis. Treatment primarily relies on clinical presentation, supported by corroborative measurements of compartmental pressure. A fasciotomy is an emergency procedure used to treat acute compartment syndrome. We describe a scenario involving a 19-years-old male, where in the diagnosis and postoperative outcome was swiftly facilitated by point-of-care ultrasound (POCUS), revealing a substantial thigh hematoma within the anterior compartment with vascular compromise before fasciotomy revealed by color and pulse wave doppler. Using POCUS, restorage of circulation and local hemodynamics after fasciotomy were assured by detecting normal doppler signal of previously involved peripheral arteries. Although POCUS should not serve as the sole method for evaluating potential compartment syndrome, it can significantly contribute as a supplementary tool in the diagnostic process and especially when following up patients where therapeutic actions have been done.
Key Words: compartment syndrome; fasciotomy; POCUS.
Introduction
Compartment syndrome arises when an enclosed muscle space in the body experiences an excessive pressure buildup, often triggered by bleeding or swelling following an injury. The relatively fixed volume inside the fascial compartments means that any introduction of excess fluid or external constriction can elevate the pressure within the compartment, subsequently impeding circulation and reducing tissue perfusion. This heightened pressure restricts blood flow and delivery of oxygen and nutrients to and from the affected tissues. Compartment syndrome manifests as an intense pain due to elevated pressure within muscles, impeding blood flow and thereby depriving nerve and muscle cells of essential oxygen and nutrients delivery. This condition is typically diagnosed clinically, often identified by the classic presentation of the 5 ‘P’s: pain, pulselessness, pallor, paresthesia and paralysis (1). Compartment syndrome may present as either acute, characterized by severe symptoms over a brief duration, or chronic, persisting over an extended period. The acute compartment syndrome stands as the predominant form of the condition, with approximately three-quarters of cases stemming from a fractured leg or arm (2). This variant swiftly progresses over hours or days until permanent damage is done, and it is considered as the most severe form. Without timely intervention, it can lead to functional impairment or necessitate amputation of the affected region. Chronic compartment syndrome, also referred to as exertional compartment syndrome, typically does not present as a medical emergency which is frequently triggered by athletic activity and is reversible through rest and relaxation (3).
Case Presentation
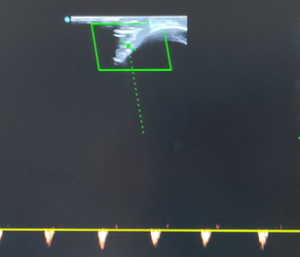
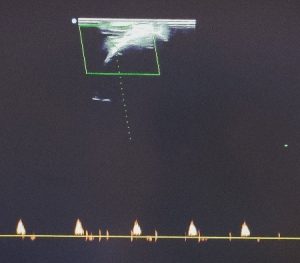
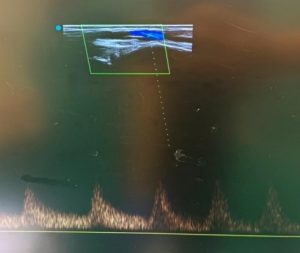
We present a case of 19 years old male, 75kg by weight and 180cm height, without history of chronic diseases and no therapy in use. Four hours before admission, he had a motorcycle accident in which he got an injury to his right lower leg, resulting with compartment syndrome. He was admitted to the University Clinic for Traumatology, Orthopedics, Anesthesia, Reanimation, Intensive Care and Emergency Department in Skopje for an urgent fasciotomy in order to prevent further damage of muscles, nerves and soft tissue due to impaired blood flow. Surgery has been conducted 4 hours and 45 minutes after injury under spinal anesthesia, a choice made with consideration of the local anesthetic vasodilatory properties on the vessels and circulation. This decision aimed to enhance post-fasciotomy perfusion, contributing to better tissue oxygenation, since preoperatively we did a color and pulse wave doppler examination where significantly low velocity with poor, nearly absent flow and retrograde diastolic blood flow were registered at arteria dorsalis pedis as shown in Figure 1A and 1B. Surgery has lasted 45 minutes. Postoperatively, in the operating room, immediately after fasciotomy, we did a Point of Care Ultrasound examination of arteria dorsalis pedis and arteria retro-malleolar using Color Doppler and Pulse Wave Doppler modalities to assure if there was present adequate blood flow and assess vascular patience. A perfect pulsation and a Doppler signal on both examined arteries has been registered with Color Doppler, as well as with Pulse wave Doppler confirming restorage of blood flow followed by elevated values for blood flow velocity with disappearance of the retrograde diastolic blood flow compared to the preoperative findings as shown at Figure 1C. Clinical examination as well has shown palpable pulses on both arteries, while warming of the injured leg has been observed too, after fasciotomy was performed. The patient has been discharged 2 days after surgery and at 1st, 3rd and 6th month of follow up after surgery had signs of complete recovery from the injury without any consequences.
Figure 1. Presence of Diastolic reverse arterial flow of arteria dorsalis pedis before fasciotomy (A) with low systolic velocity before fasciotomy (B) and restoring of blood flow with normal pulse wave signal of arteria dorsalis pedis after fasciotomy (C).
Discussion
The aim of treating compartment syndrome is to alleviate the dangerous pressure within the affected body compartment. This often involves removing any constricting dressings, casts, or splints from the affected body part. In alert patients with acute compartment syndrome, surgical intervention is typically guided by clinical assessment (2,3). The four classic signs and symptoms, often referred as the four Ps, include: pain that is out of proportion to clinical findings, pain with passive stretch of involved muscles, pain associated with palpation of involved compartment resulting from the pressure increase within the compartment (4). Absolutely, it’s essential to recognize that not all these signs may be present in cases of acute compartment syndrome. Moreover, the absence of a pulse or weak pulsation of the lower extremity arteries is more indicative for presence of significant vessel injury, typically occurring as a very late manifestation of compartment syndrome, as was previously presented in our case report (5). Since blood flow is more than essential for tissue metabolic needs of oxygen, glucose and nutrients, early recognition of blood flow impairment and vascular patency involvement may be crucial regarding establishing an on-time indication for fasciotomy and performing fasciotomy as soon as possible in order to provide better outcome (6,7). Complete recovery without any consequences have been associated with early recognition of acute compartment syndrome and performing fasciotomy within 6 hours of injury as it was presented in our case, while catastrophic complications were met in cases where fasciotomy was delayed up to 12 hours (8). In those patients who are unable to communicate pain or paresthesia, clinical examination alongside compartment pressure monitoring assumes greater significance in aiding diagnosis which could be simplified if vascular patency and current blood flow examination with doppler ultrasonography is done as well. The utilization of Point of Care Ultrasound (POCUS) needle guidance has enhanced the assessment of compartment pressures, offering a more precise approach compared to the traditional method, which relies on blind palpation and landmarks. That has been clearly described and discussed in the case report of Daniel L. et al. where needle guidance for measurement of intra-compartmental pressure was done under ultrasound guidance (9). The occurrence of limb compartment syndrome could be associated with limb fracture, or without bone fracture at all, but with significant soft tissue injury. Since clinical examination of patients with complex trauma has a low sensitivity in detecting compartment syndrome, adding complementary methods in diagnosis is recommended. Direct needle measurement of intra-compartmental pressure has been strongly recommended by the American College of Surgeons, Trauma Committee. In the study of Mc Loughlin S. et al., Pulse Wave examination of the brachial artery in patients where different levels of external pressure were added in order to mimic compartment syndrome, mean velocity and blood flow were lowered and diastolic retrograde arterial flow were observed in all groups (10). All assessed parameters have shown correlation with the grade of severity of the compartment syndrome exhibiting the worst results in the group where the pressure was the highest (10). Therefore, mean velocity, blood flow and diastolic retrograde arterial flow should be examined in all patients where compartment syndrome is suspected in order to facilitate on time diagnosis. According to Fukuda I. et al. contemporary approach of limb viability assessment implies examination of motor and sensory functions combined with interrogating Doppler flow signals at the level of the pedal arteries as categorized by Rutherford (11). Another case report of acute compartment syndrome of the limb because of burns was published by Mahmoud O. et al., where the role of doppler ultrasound examination in decision making was highlighted. In their article they had described presence of impaired blood flow and impaired doppler signals at the arteries located proximally of the compartment syndrome which are identical to our findings before performing fasciotomy (12). Compared to their case, we have examined the patient prior to operating room entrance and immediately after fasciotomy was performed which has brought us clear information about the blood flow and limb hemodynamic after performing fasciotomy showing totally different velocities and blood flow at the second examination where the ultrasound signs of altered circulation have disappeared. In another case report published by Smith A. et al., point of care ultrasound was used in diagnosis of acute compartment syndrome of the limb in a patient where the cause was a snake envenomation. They have reported that frequent ultrasound examinations in conjunction with clinical examination have aided significant data for diagnosis, following up and making a decision for fasciotomy in order to rescue the limb (13). Another study had evaluated the importance of POCUS when diagnosing acute compartment syndrome in a group of snakebite patients, where 27 patients were examined with ultrasound for locating soft tissue swelling and presence of diastolic retrograde artery flow as a sign of acute compartment syndrome. When soft tissue swelling is present, the space inside the compartment becomes reduced and at some point, leads to an artery compression exhibiting diastolic retrograde artery flow as a sign suggestive for acute compartment syndrome, which has been found in our patient before fasciotomy and have disappeared following surgical intervention (14). Eicken J. had published a case report where usage of bedside ultrasound has led to rapid diagnosis of compartment syndrome of the lower extremity in a patient taking anticoagulant therapy and experiencing symptoms of tightness of the right thigh. According to the authors immediate point of care ultrasound has led to decision for ordering further examination with CT in order to confirm the diagnosis of compartment syndrome since using ultrasound has shown a presence of right thigh hematoma with vascular compromise detected using color doppler mode, highlighting the significance of recognizing the findings associated with acute compartment syndrome (15).
Not many case reports were published nowadays, but the very few of them that were accessible at Pub Med were cited in the discussion of this article where systematic comparison of ours and their findings was done in order to provide conclusion about the usefulness of the point of care ultrasound as a diagnostic tool, but as well as an available tool for following up patients after taking therapeutic actions. If we consider the fact that in short time framework, we have performed doppler examination at two different points, through the valuable ultrasound data we could follow the evolution of the hemodynamic changes in patients with compartment syndrome. Although doppler ultrasound is still not considered as a sole diagnostic technique when establishing diagnosis of acute compartment syndrome, however it can be helpful in many ways, either for diagnosis of injured limb hemodynamic disturbances or for postoperative follow up of the vascular patency.
Conclusion
The assessment of compartment pressures benefited from POCUS needle guidance making this procedure more precise than blind intra-compartmental pressure measurement. Point of Care assessment of doppler signals of arteries located proximately to the compartment syndrome could provide significant information for the local perfusion and hemodynamics and according to us should become a standard procedure, since it is widely available and easy to perform. While it’s not advisable to rely solely on POCUS for diagnosing compartment syndrome, it can serve as a valuable adjunct in the diagnostic process, and it can also give us information for postoperative outcome. Obviously, the usage of POCUS instantly providing valuable information in critical moments could overcome the expectations of many and facilitate many aspects of treatment.
References:
- American Academy of Orthopedic Surgeons/Major Extremity Trauma and Rehabilitation Consortium Management of Acute Compartment Syndrome Clinical Practice Guideline. https://www.aaos.org/acscpg Published December 7, 2018. Accessed 04/24/2024.
- Long N, Ahn JS, Kim DJ. Adjunctive Use of Point of Care Ultrasound to Diagnose Compartment Syndrome of the Thigh. POCUS J. 2021 Nov 23;6(2):64-66. doi: 10.24908/pocus. v6i2.15185.
- Garner MR, Taylor SA, Gausden E, Lyden JP. Compartment syndrome: diagnosis, management, and unique concerns in the twenty-first century. HSS J. 2014 Jul;10(2):143-52. doi: 10.1007/s11420-014-9386-8. Epub 2014 Jun 7.
- Rauf J, Iohom G, O’Donnell B. Acute compartment syndrome and regional anaesthesia – a case report. Rom J Anaesth Intensive Care. 2015 Apr;22(1):51-54.
- Matsen FA 3rd. Compartmental syndrome. An unified concept. Clin Orthop Relat Res. 1975 Nov-Dec;(113):8-14.
- Sala-Blanch X, de Andrés J, Dewaele S. Acute Compartment Syndrome of the Limb: Implications for Regional Anesthesia. In: Hadzic A. eds. Hadzic’s Textbook of Regional Anesthesia and Acute Pain Management, 2e. McGraw-Hill Education; 2017. Accessed April 24, 2024.
- Suzuki T, Moirmura N, Kawai K, Sugiyama M. Arterial injury associated with acute compartment syndrome of the thigh following blunt trauma. Injury. 2005 Jan;36(1):151-9. doi: 10.1016/j.injury.2004.03.022.
- Fowler S.J., Symons J., Sabato S., Myles P.S. Epidural analgesia compared with peripheral nerve blockade after major knee surgery: a systematic review and meta-analysis of randomized trials. Br J Anaesth. 2008;100:154–164. doi: 10.1093/bja/aem373.
- Daniel L. Puebla, Matthew Apicella, Oren J. Mechanic, Robert A. Farrow, Point of care ultrasound needle guidance to assist diagnosis of acute gluteal compartment syndrome, The American Journal of Emergency Medicine, Volume 62, 2022, Pages 147.e5-147.e7, ISSN 0735-6757, https://doi.org/10.1016/j.ajem.2022.09.004.
- Mc Loughlin S, Mc Loughlin MJ, Mateu F. Pulsed Doppler in simulated compartment syndrome: a pilot study to record hemodynamic compromise. Ochsner J. 2013 Winter;13(4):500-6. PMID: 24357997; PMCID: PMC3865827.
- Fukuda I, Chiyoya M, Taniguchi S, Fukuda W. Acute limb ischemia: contemporary approach. Gen Thorac Cardiovasc Surg. 2015 Oct;63(10):540-8. doi: 10.1007/s11748-015-0574-3. Epub 2015 Aug 1. PMID: 26232356.
- Mahmoud OA, Mahmoud MZ. Spectral Doppler findings in a rare case of acute compartment syndrome following leg burn. Radiol Case Rep. 2018 Feb 3;13(2):352-355. doi: 10.1016/j.radcr.2018.01.006. PMID: 29904471; PMCID: PMC5999936.
- Smit A, Lalloo V, Engelbrecht A, Mashego LD, Monzon BI. Point-of-care ultrasound assessment of a swollen limb following snakebite envenomation – an adjunct to avoid fasciotomy. S Afr J Surg. 2023 Mar;61(1):14-16. PMID: 37052284.
- Ho CH, Ismail AK, Liu SH, Tzeng YS, Li LY, Pai FC, Hong CW, Mao YC, Chiang LC, Lin CS, Tsai SH. The role of a point-of-care ultrasound protocol in facilitating clinical decisions for snakebite envenomation in Taiwan: a pilot study. Clin Toxicol (Phila). 2021 Sep;59(9):794-800. doi: 10.1080/15563650.2021.1881535. Epub 2021 Feb 19. PMID: 33605805.
- Eicken JJ, Morrow D. Limb threatening thigh hematoma diagnosis accelerated by emergency physician bedside ultrasound. SAGE Open Med Case Rep. 2019 May 6;7:2050313X19848589. doi: 10.1177/2050313X19848589. PMID: 31105957; PMCID: PMC6503592.