UDK: 616.24-076-032:611.233
Golgota S1, Reveli K1, Tashi E1, Broqi M1, Papa A2, Peposhi I1, Mezini A1
1Regional Hospital Center “Shefqet Ndroqi”, Tirana, Albania
2Regional Hospital of Berati, Albania
Abstract
Introduction: Transbronchial lung biopsy is the method of choice for diagnosis of pulmonary lesions and can be used for diagnosis of a wide range of pulmonary diseases such as interstitial lung diseases, vascular diseases, small airway diseases, malignancies such as disseminated form of the alveolar cell carcinoma and infections.
Method: In this article, a clinical case presented in our department is studied. The case was consulted with online database literature (PubMed) related to problems of the diagnosis process and treatment of the pathology. The patient was treated for pneumonia at his regional hospital, but after having no improvement, he was referred to our service for further laboratory and imaging examinations.
Results: CT-Scanner of the chest suggested carcinomatous lymphangitis, without excluding primary origin and multiple lytic lesions of the skeleton. Thoracentesis of pleural fluid resulted exudate and cytology suggested a (adeno) carcinomatous process originating from upper gastro-intestinal tract, but there was no sign of malignancy in fibro-gastro-duodenoscopy. On bronchoscopy there was not seen any infiltration of airways, but after undergoing again the endoscopic procedure where transbronchial biopsy was taken. Histopathological result showed Mucinous lung adenocarcinoma. Oncologist consultation concluded Stage IV A Lung Cancer and suggested palliative care due to stroke complication.
Discussions: Data suggests higher sensitivity of transthoracic biopsy compared to transbronchial approach, especially when lesions are peripheral and less than 2cm, but with lower safety profile. As the success of a diagnostic test should result from a proper balance between accuracy and procedure-related complications, transbronchial approach has been shown to have a better safety profile.
Conclusions: Compared with open lung biopsy, transbronchial biopsy has lower morbidity and mortality. Transbronchial biopsy is indicated in the following settings: neoplastic disease, suspected sarcoidosis or hypersensitivity pneumonitis, interstitial lung disease, pulmonary infection, or unusual and unclear lung disease.
Key Words: lung cancer, diagnosis, transbronchial biopsy.
Introduction
Lung cancer is one of the leading causes of cancer-related deaths. The increasing use of high-quality CT in daily medical practice has increased the number of lung lesions discoveries incidentally, mostly peripheral lung lesions. The gold standard for a diagnosis of lung cancer remains pathological data. Flexible bronchoscopy, transthoracic needle aspiration and surgical biopsy are also available, and transbronchial biopsy with a bronchoscope is the most generally accepted method for diagnosing malignant pulmonary lesions.
Transbronchial lung biopsy is the method of choice for diagnosis of pulmonary lesions and can be used for diagnosis of a wide range of pulmonary diseases such as interstitial lung diseases, vascular diseases, small airway diseases, malignancies such as disseminated form of the alveolar cell carcinoma and infections.
An increasing number of pulmonary lesions, particularly lung lesions that don’t infiltrate bronchial airways, are identified with current technological advancements. Notably, the yield of traditional bronchoscopy for the diagnosis of peripheral lung lesions is low.
Methods and Results
In this article, a clinical case presented in our department is studied. The case was consulted with online database literature (PubMed) related to problems of the diagnosis process and treatment of the pathology. The patient was treated for pneumonia at his regional hospital, but after having no improvement, he was referred to our service for further laboratory and imaging examinations.
Our 38-years-old male patient was diagnosed and treated as pneumonia at his regional hospital, but after having no improvement, he was transferred for further diagnosis at our hospital.
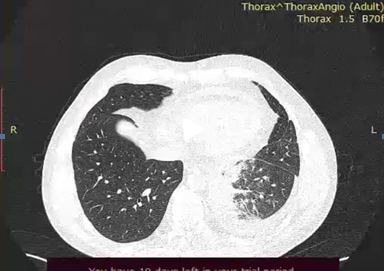
Computerized tomography suggested carcinomatous lymphangitis, without excluding primary origin and multiple lytic lesions of the skeleton. The radiologist suggested endoscopic examination.
Figure 1. CT images of lungs where carcinomatous lymphangitis was suggested.
Thoracentesis of pleural fluid resulted exudate and cytology
suggested a (adeno) carcinomatous process originating from upper gastro-intestinal tract.
Figure 2. Pleural effusion sample taken at the emergency unit.
On bronchoscopy there was not seen any infiltration of airways.
Fibro-gastro-duodenoscopy showed superficial gastro-duodenitis.
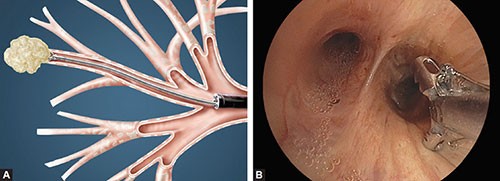
Patient underwent again the endoscopic procedure where transbronchial biopsy was taken.
Figure 3. Endoscopic procedure where transbronchial biopsy was taken.
Histopathological result showed Mucinous lung adenocarcinoma.
During hospitalization, the patient started having difficulties speaking leading to aphasia. Head CT resulted with multiple ischemic lesions.
Figure 4. Head CT showed multiple ischemic lesions.
Neurologist and neuro-surgeon consultation: Ischemic stroke due to malignant disease.
Oncologist consultation concluded Stage IV A Lung Cancer and suggested palliative care due to stroke complication. The patient left hospital and passed away two weeks later at his home.
Discussion
Endoscopic bronchial procedures are used to visualize the tracheobronchial tree and obtain specimens of abnormal lesions. However, small and peripheral lung lesions are difficult to diagnose with these procedures, thus further improvement is desired in the diagnostic efficacy of bronchoscopy for lesions not affecting bronchial airways.
Data suggests higher sensitivity of transthoracic biopsy compared to transbronchial approach, especially when lesions are peripheral and less than 2cm, but with lower safety profile. As the success of a diagnostic test should result from a proper balance between accuracy and procedure-related complications, transbronchial approach has been shown to have a better safety profile.
Conclusions
Our clinical case enhances the importance of endoscopic examinations for the diagnosis of lung cancer. Transbronchial biopsy is very useful for taking samples from pulmonary lesions. Compared to open lung biopsy, trans-bronchial biopsy has lower morbidity and mortality. Transbronchial biopsy is indicated in the following settings: neoplastic disease, suspected sarcoidosis or hypersensitivity pneumonitis, interstitial lung disease, pulmonary infection, or unusual and unclear lung disease.
It should be mentioned that trans-bronchial biopsy is not always done without complications. And local anesthesia is mostly used for patients undergoing this procedure. Regarding to our case, patient did not have any complication during and after procedure.
References
- Nasim F, Sabath BF, Eapen GA. Lung Cancer. Med Clin North Am. 2019 May;103(3):463-473. doi: 10.1016/j.mcna.2018.12.006. PMID: 30955514.
- Nooreldeen R, Bach H. Current and Future Development in Lung Cancer Diagnosis. Int J Mol Sci. 2021 Aug 12;22(16):8661. doi: 10.3390/ijms22168661. PMID: 34445366; PMCID: PMC8395394.
- Dubey AK, Gupta U, Jain S. Epidemiology of lung cancer and approaches for its prediction: a systematic review and analysis. Chin J Cancer. 2016 Jul 30;35(1):71. doi: 10.1186/s40880-016-0135-x. PMID: 27473753; PMCID: PMC4967338.
- Kurihara Y, Tashiro H, Takahashi K, et al. Factors related to the diagnosis of lung cancer by transbronchial biopsy with endobronchial ultrasonography and a guide sheath. Thorac Cancer. 2022 Dec;13(24):3459-3466. doi: 10.1111/1759-7714.14705. Epub 2022 Oct 20. PMID: 36263938; PMCID: PMC9750813.
- Chugh K, Jatwani S. Transbronchial biopsy vs. bronchoalveolar lavage in interstitial lung disease. Curr Opin Pulm Med. 2022 Jan 1;28(1):3-8. doi: 10.1097/MCP.0000000000000847. PMID: 34750299.
- Pajares V, Núñez-Delgado M, Bonet G, et al; MULTICRIO Group researchers. Transbronchial biopsy results according to diffuse interstitial lung disease classification. Cryobiopsy versus forceps: MULTICRIO study. PLoS One. 2020 Sep 21;15(9):e0239114. doi: 10.1371/journal.pone.0239114. PMID: 32956379; PMCID: PMC7505587.