UDK: 618.3-06:616.12-008.331.1
https://www.doi.org/10.55302/MJA2484153j
Jovcheva L1, Eftimova B1, Buntashevska B2
1 Faculty of Medical Sciences, “Goce Delchev” University, Shtip, Republic of North
Macedonia, Medical School – Second cycle studies – medical nurse specializing in
intensive care
2University Clinic for Traumatology, Orthopedic Diseases, Anesthesiology, Reanimation and Intensive Care Medicine and Emergency Department, Clinical Center “MotherTheresa” Faculty of Medicine, “Ss. Cyril and Methodius” University, Skopje, Republic of North Macedonia
Abstract
Hypertensive disorders are the most common medical complications that can occur during pregnancy, with an incidence ranging between 5–10%. These disorders are the leading cause of maternal mortality worldwide.
Objective: The aim of this retrospective study is to analyze the two-years archives data of the University Clinic of Gynecology and Obstetrics (UC OF G&OB) at the Clinical Center “Mother Teresa” – Skopje, concerning the hypertensive disorders during pregnancy, and to determine the main causes for its development, as well as the potential for their prevention.
Materials and Methods: The methodology used for the development of this specialist paper is primarily research-based and analytical. The analytical approach is based on data obtained from the Archives of the UC OF G&OB. The research approach included survey interviews designed for gynecologists, which were conducted with 4 gynecologists. The survey consisted of several open-ended questions.
Results: The research concluded that gestational hypertension the most often appears in, or after the 37th gestational week. Severe forms of hypertensive diseases during pregnancy include preeclampsia, eclampsia and HELLP syndrome. Preeclampsia occurs in 2-7% of the cases, and it is the most common disorder in women pregnant for the first time. Obesity is a definitive risk factor for preeclampsia, and the risk increases as the body mass index rises, especially in pregnant women who gained 1kg per week during the third trimester.
Conclusions: The doctor or nurse who refers to the patient should consult with the physician at the perinatal center regarding the referral and appropriate treatment. All data regarding the severity of the case, including prenatal information and a detailed medical record, should be sent along with the patient. Blood pressure should be stabilized, and convulsions should be controlled.
Keywords: hypertension; pregnancy; gestational week.
Introduction
Hypertension complicates approximately 7-10% of all pregnancies (1). It is much more common in the first-time mothers than in multiparas. The term hypertension in pregnancy is used to describe a broad spectrum of conditions, ranging from mild increases in blood pressure to severe forms of hypertension with various types of organ damage and dysfunction (2). The manifestations in these patients may be presented with similar clinical features, such as hypertension and proteinuria. However, they may stem from different causes, including chronic hypertension, kidney insufficiency or pure preeclampsia. The three most common forms of hypertension in pregnancy are acute gestational hypertension, preeclampsia and chronic essential hypertension (3).
Hypertension may preexist before pregnancy or may be diagnosed for the first time during pregnancy. Chronic hypertension is defined as hypertension that exists before pregnancy or is diagnosed for the first time before the 20th gestational week. Hypertension that persists 42 days after delivery is also classified as chronic hypertension.
Gestational hypertension is the most common cause of hypertension during pregnancy, with an incidence ranging from 6 to 17%, and it significantly increases in multiple pregnancies (4).
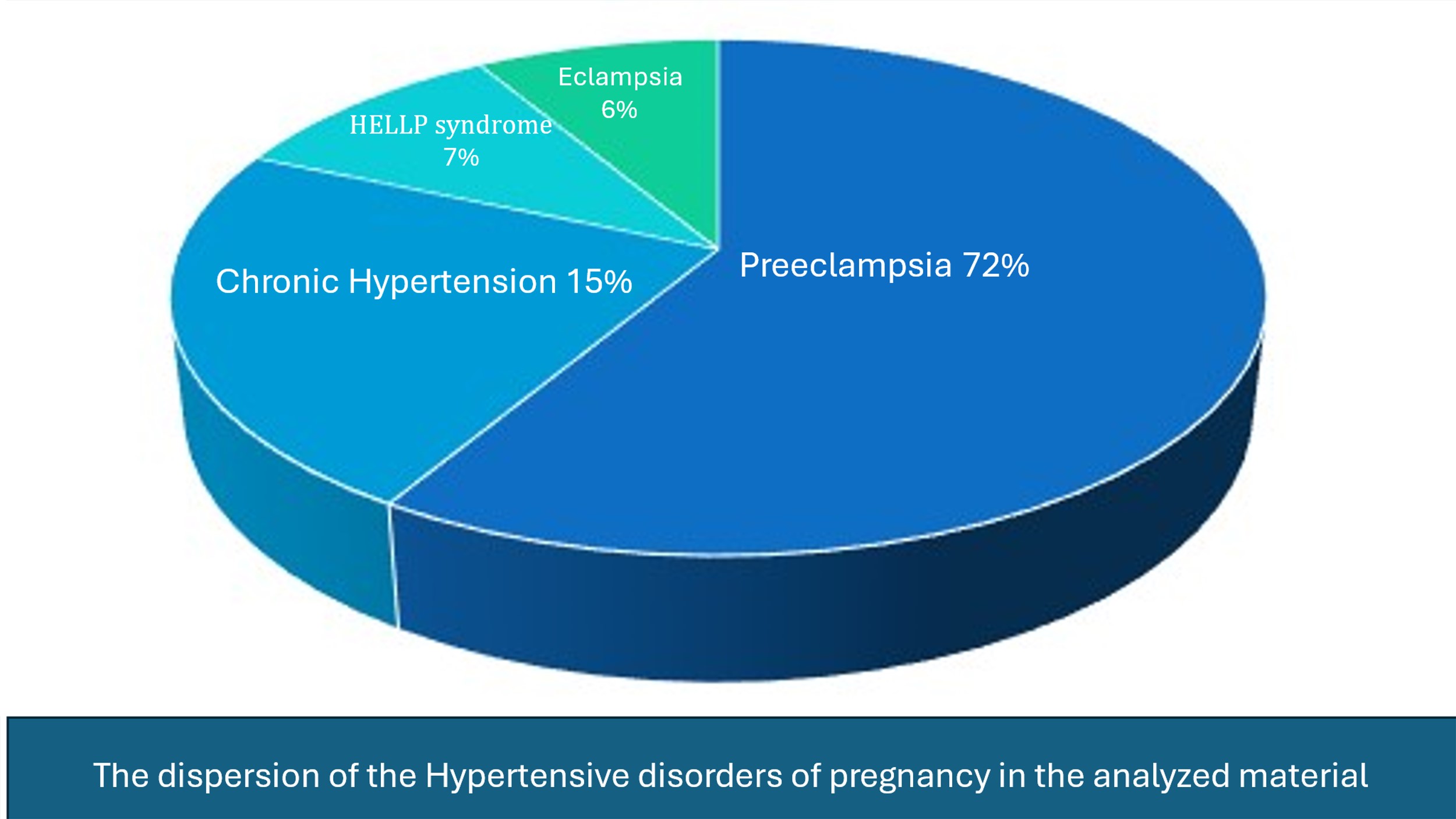
Preeclampsia accounts for about 70% of all cases of hypertensive complications during pregnancy.
Hypertensive complications during pregnancy represent a broad spectrum and can have either minimal consequences for the mother and fetus or pose life-threatening conditions for both. Mild or moderate preeclampsia that occurs toward the end of pregnancy carries a low risk of hypertension in the next pregnancy. Severe preeclampsia, which occurs in the early stages of pregnancy, around the 28th week of gestation, presents a high risk for the woman to develop serious hypertensive complications in the next pregnancy.
There are many terms and phrases used to describe hypertensive complications during pregnancy, to the point that specialists from different regions of the world may not fully understand each other during conversations. These differences complicate the interpretation of results from various studies. These disorders were once referred to as “toxemia of pregnancy” or “pregnancy toxemia,” as it was believed to be caused by a circulating toxin. However, no such toxin has been discovered to date, so this term has been abandoned and lacks scientific foundation for its use. J. Roberts (1989, Book No. 20, p. 777) defines the term “pregnancy toxemia” as archaic, stating that it neither describes the disease nor clarifies its etiology and should reasonably be discarded (4).
The American College of Obstetricians and Gynecologists (ACOG) classifies hypertensive complications (HC) of pregnancy as follows (Table 1). (5)
Table 1. Hypertensive disorders of pregnancy.
- Chronic hypertension
- Gestational hypertension
- Preeclampsia/eclampsia
- Chronic hypertension with superimposed preeclampsia/eclampsia
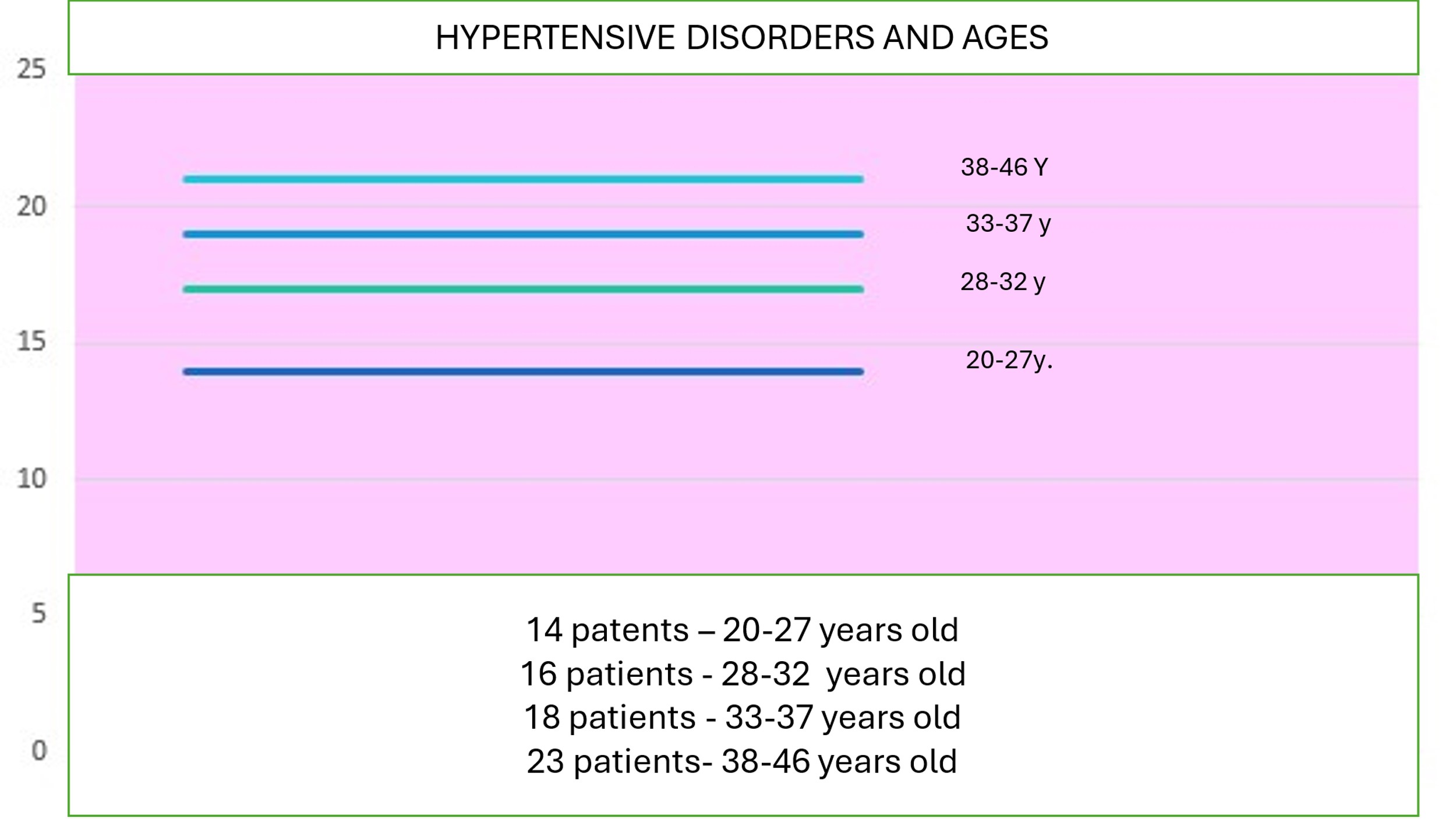
The age of the pregnant women is the key factor of risk for development preeclampsia, the age under 15, is 2.5 times greater than in women aged 30-34 years. The risk also increases after the age of 35. A history of preeclampsia in a previous pregnancy significantly increases the risk of developing preeclampsia in the next pregnancy (odds ratio +10.8), i.e., it is 10 times more likely. Women with increased body weight (odds ratio +2.7), women who work during pregnancy, and women with a family history of hypertensive diseases are also at increased risk. When a woman has a spontaneous abortion, the chances of developing preeclampsia in the subsequent pregnancy decrease (6,7).
The second reason for high blood pressure during pregnancy is mostly caused by an unhealthy lifestyle and diet during pregnancy, particularly a diet high in salt, physical inactivity and many other factors. Untreated preeclampsia can lead to eclampsia, which is one of the most severe pregnancy disorders that can result in death for both the baby and the mother. The global mortality rate for eclampsia is 3% (8).
The diagnosis of eclampsia is confirmed when the following criteria are met – general edema, proteinuria, hypertension and convulsions. Hypertension is considered a hallmark in the diagnosis of eclampsia. It can be severe (systolic blood pressure of at least 160mmHg and diastolic blood pressure of at least 110mmHg), which occurs in 20 to 54% of cases, or mild (systolic blood pressure between 140 and 160mmHg, diastolic blood pressure between 90 and 110mmHg), which occurs in 30 to 60% of cases. Several clinical symptoms can help in the diagnosis of eclampsia, including persistent occipital and frontal headaches, blurred vision, photophobia, epigastric pain, or pain in the upper right quadrant, as well as altered mental status (9).
The motivation for this research and writing this specialist paper is primarily personal, arising from the still-high rate of pregnant women with preeclampsia, and more rarely with eclampsia and HELLP syndrome.
We have formulated a hypothesis: “The majority of preeclampsia cases are associated with hypertension, obesity and older pregnant women.”.
Objectives of the Study
The aim of this retrospective study is to analyze the two years archives data of the University Clinic of Gynecology and Obstetrics (UC OF G&OB) at the Clinical Center “Mother Teresa” – Skopje, concerning the hypertensive disorders during pregnancy, and to determine the frequencies of the HC, main causes for development of HC, and to discuss the potential for their prevention.
Material and Method
This is a retrospective analytical study conducted at the University Clinic of Gynecology and Obstetrics at the Clinical Center – Skopje, where the archive materials for two-years period from 01.01.2022 to 31.12.2023 were studied. The study was a survey interview with gynecologists (involving 4 gynecologists). The survey consisted of several open-ended questions.
The obtained data will be presented in tabular and graphical form, followed by an analysis of the data to draw conclusions.
Results
The data presented in this specialist paper were obtained under archive number (04 – 1463/1 from 21.10.2024).
During this period, a total of 64 patients with developed preeclampsia were hospitalized at the Department of Gynecology and Obstetrics. The patients were from all over the country. All patients had hypertension >140/90 mm/Hg, some had proteinuria and facial edema.
A statistical analysis was conducted, covering 71 patients. Out of these patients, 48 were primigravids (first-time pregnancies), making up 68% of the total number of hospitalized patients; 3 were pregnant with multiple fetuses (4%), and 20 patients were in their second pregnancy (28%).
The distribution of the type of hypertensive complication is presented in Figure 1.
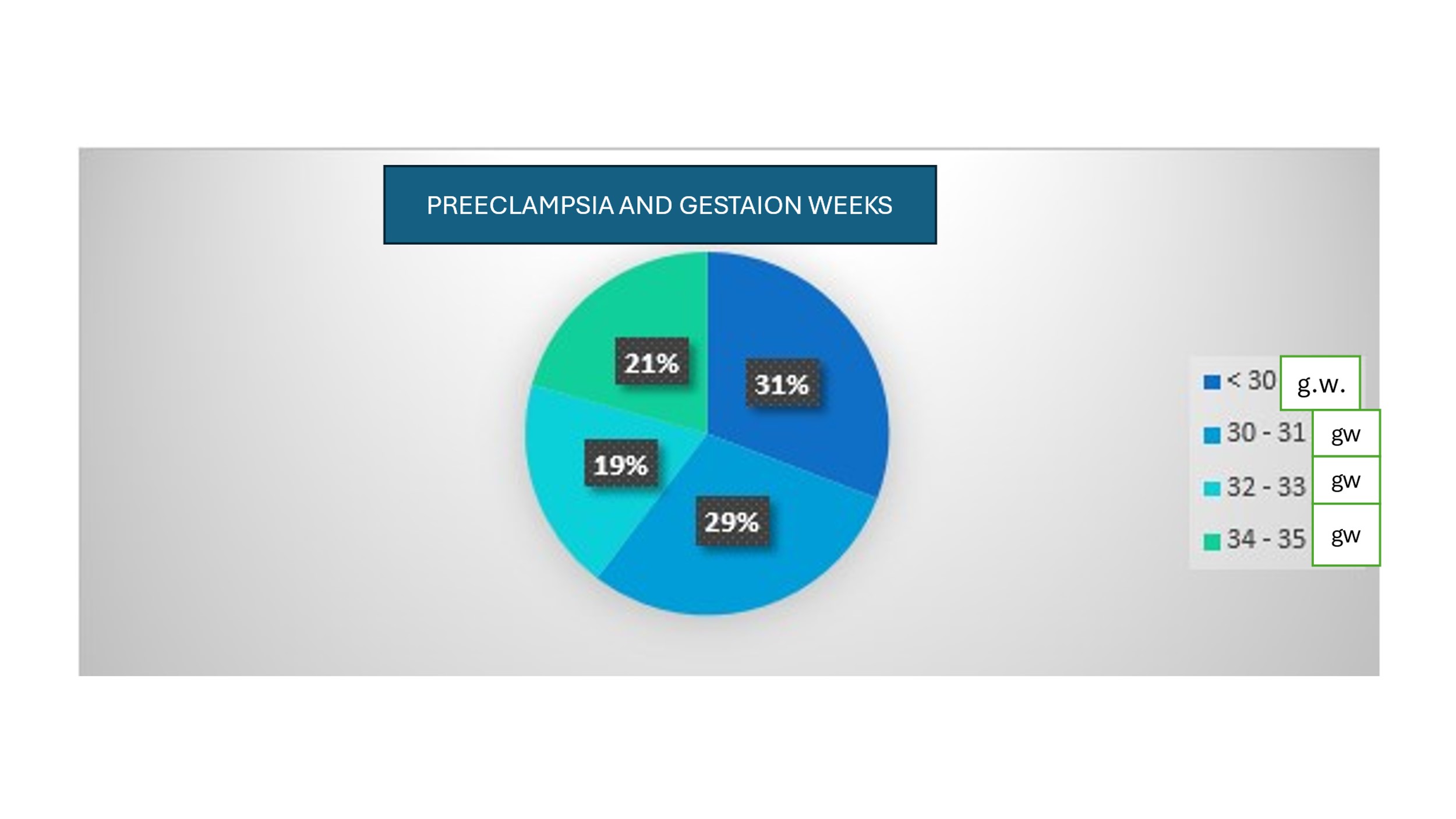
Figure 1. A graphical presentation of patients with preeclampsia who were hospitalized at University G&OB Clinic Skopje is provided (Figure 2).
Figure 2. Percentage of the pregnant women with preeclampsia in the gestation weeks.
The data were processed according to the age of the patients, the number of pregnancies, and a survey about how many of them had a family history of hypertension during pregnancy (Fig. 3).
Figure 3. Hypertensive complications in analyzed materials.
Discussion
The treatment of such patients involves hospitalization for the remainder of the pregnancy due to the knowledge that hospital care reduces the possibility and frequency of progression to severe disease and allows for quick intervention in cases of sudden worsening, such as the development of abruptio placentae, eclampsia or hypertensive crises (10,11,12). However, these complications are becoming increasingly rare, as we live in a time when women’s awareness of the importance of regular gynecological checks during pregnancy is rising. Therefore, even if there is some disturbance, it would be detected in time and treated accordingly. Moreover, results from studies on women with gestational hypertension, selected randomly, and several studies observing women with mild hypertension and mild preeclampsia, suggest that most of these women can be safely treated at home or in a day-care center, provided they undergo frequent checks of their condition and their fetus’s condition (13,14,15,16). It must be noted that many of the women included in this study had only gestational hypertension before developing any serious condition. Continuous rest for the remainder of the pregnancy is often recommended for pregnant women with mild hypertension. However, no concrete evidence has been found that such a practice improves pregnancy outcomes. Furthermore, no published studies of randomly selected women compare continuous bed rest with physical activity limitation in treating mild preeclampsia. On the other hand, prolonged bed rest during the remainder of pregnancy increases the risk of thromboembolism.
The social and scientific justification for this thesis is based on the methodology used, which ensures that recommendations from specialists (gynecologists) for easier prevention and control of eclampsia during pregnancy are provided. The social and professional justification for this topic arises from the importance of raising awareness among pregnant women, especially those with previous risk factors for developing a pathological condition related to pregnancy, such as preeclampsia, eclampsia and HELLP syndrome. The goal is timely intervention and symptom recognition to minimize the incidence of these diseases and, in the worst cases, reduce mortality (17).
Conclusion
The hypertensive disorders during pregnancy still stays an actual topic in our country. The prevention of the hypertension and primary care of the pregnant women is the main moto to decrease the incidences of complications. The doctor or nurse who refers to the patient should consult with the physician at the perinatal center regarding the referral and appropriate treatment. All data regarding the severity of the case, including prenatal information and a detailed medical record, should be sent along with the patient. Blood pressure should be stabilized, and convulsions should be controlled.
Acknowledgements:
The author of this paper would like to thank Professor Dr. Biljana Eftimova for her help and guidance in the preparation of this paper.
References:
- Report of the National High blood Presure Education program. Working group Report on high blood pressure in Pregnancy. Am J Obstet gynecol 2000; 183: S1.
- Sibai BM. Diagnosis and Menagement of gestational hypertension and preeclampsia. Obsest Gynecol 2003; 102 :181.
- Hauth JC, Ewell MG, Levine RL, et at: Pregnancy outcomes in healthy nulliparas women who subsequently developed hypertension. Calcium for preeclampsia prevention study group. Obstet Gynecol 2000; 95:24.
- Barton JR, O’Brien JM, Bergauer NK,et al : Mild gestational Hypertension remote from term : progression and outcome. Am J Obstet Gynecol 2001; 184 :979.
- ACOG Committee on Obstetric Practice. ACOG practice bulletin. Diagnosis and management of preeclampsia and eclampsia. Number 33, January 2002. American College of Obstetricians and Gynecologists. Int J Gynaecol Obstet. 2002 Apr;77(1):67-75. PMID: 12094777.
- Caritis S, Sibai B, Hauth J, et al: Low dose aspirin to prevent preeclampsia in women at high risk. N Engl J Med 1998; 338 :701.
- Knuist M, Bonsel GJ, Zondervan HA, Treffers PE: Intensification of fetal and maternal disorders. Int J Gynecol Obstet 1998; 61 :127.
- Lin L, August P. Genetic thrombophilia’s and preeclampsia: a meta-analysis. Obstet Gynecol 2005; 105 :182.
- O’ Brien TE, Ray JG, Chan WS: Maternal body mass index and risk of preeclampsia: a systematic overview, Epidemiology 2003; 14 :368.
- Audibert F, Friedman SA, Frangieh AY, Sibai BM: Clinical utility of strict diagnostic criteria for the HELLP (hemolysis, elevated liver enzymes, and low platelets) syndrome. Am J Obstet Gynecol 1996; 175:460.
- Haddad B, Barton JR, Livingston JC, et al: Risk factors for adverse maternal outcomes among women with HELLP (hemolysis, elevated liver enzymes, and low platelet count) syndrome. Am J Obstet Gynecol 2000; 183:444.
- Van Pampus MG, Wolf H, Westenberg SM, et al: Maternal and perinatal outcome after expectant management of the HELLP syndrome compared with preeclampsia without HELLP syndrome. Bur J Obstet Gynecol 1995; 102:111.
- Abramovici D, Friedman SA, Mercer BM, et al: Neonatal outcome in severe preeclampsia at 24 to 36 weeks’ gestation. Does HELLP Chemolysis, elevated liver enzymes, and low platelet count) syndrome matter? Am J Obstet Gynecol 1999; 180:221.
- Barton JR, Sibai BM: Diagnosis and management of HELLP syndrome. Clin Perinatol 2004; 31 :807.
- Loureiro R, Leite CC, Kahhale S, et al: Diffusion imaging may predict reversible brain lesions in eclampsia and severe preeclampsia: Initial experience. Am J Obstet Gynecol 2003; 189:1350.
- MacKay AP, Berg CJ, Atrash HK: Pregnancy-related mortality from preeclampsia and eclampsia. Obstet Gynecol 2001; 97:533.
- Khedagi AM, Bello NA. Hypertensive Disorders of Pregnancy. Cardiol Clin. 2021 Feb;39(1):77-90. doi: 10.1016/j.ccl.2020.09.005. Epub 2020 Nov 2. PMID: 33222817; PMCID: PMC7720658.