UDK: 618.25-06:618.333
https://www.doi.org/10.55302/MJA2484113l
Livrinova V1, Simeonova Krstevska S1, Kamilovska M1, Dimitrovska R1, Karadjova D1
1University Clinic for Obstetrics and Gynecology in Skopje, Faculty of Medicine, “Ss. Cyriland Methodius” University of Skopje
Abstract
Triples pregnancies is when three fetuses are carried and delivered by mother at once. The overall incidence is 1of 7,300 pregnancies. As a result of the use of aided reproductive technology, the overall incidence of these pregnancies has increased. They are with increased perinatal risks because of intrauterine growth restriction, fetal discordance, intrauterine demise, congenital malformations, preterm birth, pre-eclampsia, gestational diabetes, anemia, risk for thrombosis, operative and anesthesiology complications.The main goal of this case report is presenting the implications of intrauterine dead of two fetuses in triplets conceived spontaneously at 25 gestational weeks. It was the second pregnancy after the earlier cesarean section. The ultrasound scan at our clinic revealed diamniotic, dichorionic pregnancy with fused placentas at 23 gestational weeks with three live discordant fetuses more than 20% between them with amount of amniotic fluid in normal range. At the next control scan two weeks later, one fetus was dead and after 4 days the other one died in the same amniotic sac. In 26th gestational week, iatrogenic premature delivery with second cesarean section in regional anesthesia was done. A vital male fetus with 1,050g and 31cmand two dead fetuses were delivered.The discordance between them was 9.2% and it was 40% with a live fetus. After 10 weeks the live newborn was discharged without serious sequels. It can be concluded that it is especially important to detect multi fetal pregnancy as soon as possible, especially number of fetuses, chorionicity and amnionicity, to prevent the above-mentioned complications.
Keywords: demise; fetal; implication; maternal; triplets.
Introduction
According to Helin’s law for multiple pregnancies, the incidence of twins is 1of 86 pregnancies, triplets 1 of 862 and quadruplets 1 of 863 (1).The incidence of multiple gestations has increased in recent years due to aided reproductive technologies. Triplets and other multiple gestations are associated with increased risks of maternal and neonatal morbidity compared to singleton gestations. Premature deliveries before 34 gestational weeks (g.w.) are around 75% in triplet, 20% of twin pregnancies compared to 2 percent of singleton pregnancies (2). Diagnosis of multiple pregnancies is based on ultrasound examination, performed for confirming of fetal cardiac activity and gestational age. Generally recommended route of delivery is with the cesarean section avoiding the vaginal birth. Primary, determination of the number of placentas and amniotic sacs should be performed between 8 and 13 weeks of gestation. This is important for risk assessment, antenatal counseling, further management and for screening for congenital anomalies, labeling the fetuses, the sites of placental implantation and sharing, the sites and types of placental cord insertion. The shared amniotic sacin monochorionic monoamniotic or dichorionic diamniotic tripletsis important risk factor for fetuses for cord entanglement and twisting with later death from cord compression. It is suggested to have hospital admission with this type of placentation at 26 weeks of gestation to help performance of one hour of continuous fetal heart rate watching every eight hours (3).Triplet pregnancies are also with the higher risk for gestational diabetes compared to singletons (12.8 versus 2.9 percent respectively) (4).
Case Presentation
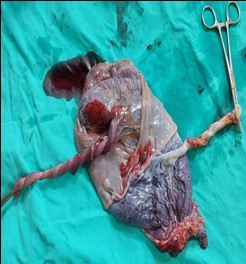
The patient was 32 years old women with her second pregnancy conceived spontaneously. The first pregnancy was at-term with the cesarean section because of Fetal distress. An ultrasound was preformed, and surprisingly for her, the tree fetuses are detected. Till that scan, she knew that she was carrying two babies. The ultrasound scan at our clinic revealed diamniotic, dichorionic pregnancy with fused placentas at 23 gestational weeks (g.w.) with alive three fetuses.The discordance of more than 20% existed between two fetuses with sheared placenta and the fetus in another sac, with amount of amniotic fluid in normal range. The fetal dopplers were in normal range. Two weeks later, the first fetus died with biometry for 23 g.w., and after 4 days the other one in the same amniotic sac. She was admitted to hospital at 25.4 g.w. and administered with corticosteroid for fetal lung maturation. In 26th gestational week, iatrogenic premature delivery with second cesarean section in regional anesthesia was done. Before delivery proper preparations measure for delivery from anesthesiology aspects to prevent complication was done. A vital male fetus with 1,050g and 31cm with Apgar Score of 6 and 7(in first and fifth minute) was delivered. Both dead fetuses were male and weighted 650g and 590g with length 28cm and 27cm respectively (Picture 1).
Picture 1. Two intrauterine died fetuses, one hydropic with twisted umbilical cords.
The fetus who died first was hydropic with maceration, the second shown sign of recent dead. Postnatal discordance between them was 9.2% and it was 40 % with a live fetus. The placentas macroscopic was with obvious demarcation line at its maternal site andthe margins of both placentas could be distinguished (Picture 2).
Picture 2. Maternal site of placenta Picture 3.Fetal site of placenta
with with clear border of placentas.membrane and insertions of umbilicals cord.
On the fetal site of placenta, there was an interesting twisting of umbilical cords of both fetuses in the same amniotic sac with common insertion of umbilical cord of dead fetuses (Picture 3). After 10 weeks the newborn was discharged with neonatal weight of 1,900g and 46cm length, without serious sequels, but during hospitalization at NICUa large and various necessary interventions were done. During operation, there was a need for administration of uterotonic-20 i.e., Oxytocin and intramuscular application of prostaglandins due to uterine delay contraction to prevent blood loss. Postoperatively antibiotics, uterotonic and thromboprophylaxis were administered. The woman was discharged on the third postoperative day without early complication in stabile state.
Discussion
Almost 80 percent of triplet and order multiple pregnancies are result of aided reproductive technology (ΑRΤ) (5). There is a risk for maternal health, especially for the heart because there is volume overload as pregnancy advance. So, in one study of triplet pregnancies, maternal median peak cardiac output was 8.44L/min and occurred at 32 to 36 weeks, while in singleton pregnancies was 6.1L/min at the same gestational age (6). There is the need for exact balance of liquid intake to prevent congestive heart failure and pulmonary edema. The risk for deep venous thrombosis and thromboembolic events is higher because of pelvic and leg veins compression of overdistended uterus. Neuraxial anesthesia is recommended for operative delivery or vaginal complicated delivery.
Gestational age of delivery for triplets is approximately 32 weeks versus 39 weeks in singletons. Because of pregnancy complications, there is common hospitalization before delivery. The most uneventful complication for fetuses is fetal demise. The rate of fetal demise after 22 weeks of gestation is related to chorioamnionitis. Fetal demise occurred in 0.8 percent of trichorionic triplet pregnancies versus 2.7 percent of monochorionic tri amniotic triplet pregnancies (7). None of the studies has exactly examined the outcomes of survivors of co-triplet demiseand this risk depends on whether they shared a chorionic sac with the demised triplet. In cases where there is demise of one or two triplets with monochorionic placentation, injury to the surviving fetus or fetuses occurs very soon. Because of this fact, the immediate delivery will not prevent adverse outcomes related to this event (8).
Perinatal mortality was approximately 2.5 percent (7,9) and monochorionic triplet pregnancies had a 2.6-fold greater risk of perinatal death than tri chorionic triplet pregnancies (7). In a study comparing dichorionic to trichorionic triplet gestations, the neonatal death rates were 22 and 7 percent, respectively, and the median gestational age at delivery was 31 and 33 weeks, respectively (10).
Conclusions
For monitoring triplet pregnancies, there is need for more ultrasound examination to recognize complications, congenital anomalies and twin-twin transfusion syndrome. Preterm birth is the most common cause of death and morbidity in triplet gestations. Iatrogenic preterm birth is usual in triplets. Compared to dichorionic survivors of a co-twin fetal demise, monochorionic survivors of a co-twin fetal demise have higher rates of later demise, preterm birth and neurodevelopmental impairment. Multiple gestations are at increased risk for uterine atony, postpartum hemorrhage and emergency hysterectomy, so preparation for these potential complications is important. There is no triplet pregnancy without implications for each one – fetus and for the mother.
References:
- Fellman, Johan; Eriksson Aldur W. “Statistical analyses of Hellin’s law”. Twin Research and Human Genetics. Apr 2009; 12 (2): 191–200.
- Osterman MJK, Hamilton BE, Martin JA, et al. Births: Final Data for 2021. Natl Vital Stat Rep 2023; 72:1.
- Kawaguchi H, Ishii K, Yamamoto R, et al. Perinatal death of triplet pregnancies by chorionicity. Am J ObstetGynecol 2013; 209:36. e1.
- Lopes Perdigao J, Straub H, Zhou Y, et al. Perinatal and obstetric outcomes of dichorionic vs Tri chorionic triplet pregnancies. Am J ObstetGynecol 2016; 214:659.
- Kulkarni AD, Jamieson DJ, Jones HW Jr, et al. Fertility treatments and multiple births in the United States. N Engl J Med 2013; 369:2218.
- Ladhani NN, Milligan N, Carvalho J, et al. Maternal hemodynamic changes in multiple gestation pregnancy: a longitudinal, pilot study. Am J ObstetGynecol 2013; 209: S104.
- Kawaguchi H, Ishii K, Yamamoto R, et al. Perinatal death of triplet pregnancies by chorionicity. Am J ObstetGynecol 2013; 209:36. e1.
- Levy-Coles M, Erez O, Mizrakli Y, et al. The effect of chorionicity on maternal and neonatal outcomes in triplet pregnancies. Eur J ObstetGynecolReprod Biol 2024; 296:200.
- Mol BW, Bergenhenegouwen L, Velzel J, et al. Perinatal outcomes according to the mode of delivery in women with a triplet pregnancy in The Netherlands. J Matern Fetal Neonatal Med 2019; 32:3771.
- Karageyim Karsidag AY, Kars B, Dansuk R, et al. Brain damage to the survivor within 30 min of co-twin demise in monochorionic twins. Fetal DiagnTher 2005; 20:91.