UDK: 616-089.5-032:611.23]-06:616.24-008.4
https://www.doi.org/10.55302/MJA2484093gb
Gavrilovska Brzanov A1, Petrusheva Panovska A1, Jovanovski Srceva M1, Brzanov N1, Nastasovic T2, Kuzmanovska B1
1 University Clinic for Traumatology, Orthopedic Disease, Anesthesiology, Reanimation and Intensive Care Medicine and Emergency Department, Clinical Center “Mother Theresa”, Faculty of Medicine, “Ss. Cyril and Methodius” University, Skopje, Republic of North Macedonia
2Neurosurgery Clinic, Department of Anesthesiology and Resuscitation, University Clinical Center of Serbia, Belgrade, Serbia
Abstract
Introduction: The three primary causes of compression and absorption atelectasis after general endotracheal anesthesia are dyskinesia, dyspnea and elevation in FIO2. General anesthesia eliminates the sigh reflex in all patients, resulting in atelectasis occurring rapidly. Alveolar recruitment maneuvers improve gas exchange, increase arterial oxygenation, and draw in collapsed alveoli. There is a wealth of literature supporting alveolar recruitment movements, and these days, mechanical ventilator settings include alveolar recruitment maneuvers. Our study’s objective was to assess the effectiveness of alveolar recruitment techniques incorporated in the GE Healthcare Carestation 750.
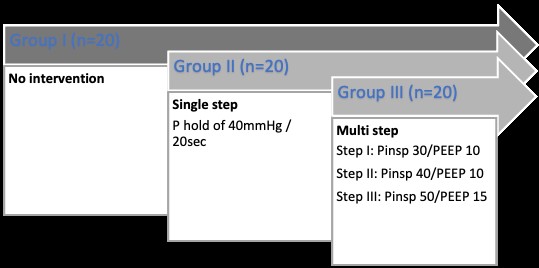
Material and Methods: This evaluation covered all ASA I-III patients between the ages of 18 and 60 who were scheduled for general endotracheal anesthesia and did not have a history of cardiac or respiratory illness. Following tracheal intubation and the onset of general anesthesia, the patients were split into three groups: Group I – no intervention; Group II – single-step recruitment (pressure hold of 40mmHg for 20 seconds); Group III – multiple-step recruitment (Step I: Pinsp 30/PEEP 10; breathes 3; Step II: Pinsp 40/PEEP 10; breaths 3; Step III: Pinsp 50/PEEP 15; breaths 3). Changes in pulmonary compliance were the main result, and variations in PaO2 and PaO2/FIO2 were the secondary result. Analyses of arterial blood gas were taken both prior to and during the recruitment maneuver. A 50% FiO2 ratio was used.
Results: There were 75 patients in total for this evaluation. In contrast to the control groups, the alveolar recruitment maneuver groups exhibited greater pulmonary compliance (37% vs. 24% Group III vs. Group II). The groups that were also given alveolar recruitment strategies experienced an increase in intraoperative PaO2 (P<0.05). Compared to the control groups, PaO2/FIO2 rose in the alveolar recruitment maneuver groups. During or after the alveolar recruitment operations, none of the patients experienced any problems.
Conclusion: The individuals undergoing the alveolar recruitment maneuver groups had improved oxygenation.
Keywords: alveolar collapse; mechanical ventilation; multi-step recruitment; single step recruitment.
*Parts of this text were published in: Gavrilovska Brzanov A., Petrusheva Panovska A., Jovanovski Srceva M., Brzanov N., Nastasovic T., Kuzmanovska B. Single-step, multi-step, or no alveolar recruitment maneuver? EJA 2024;41(62):533.
Introduction
General endotracheal anesthesia, routine practice in various surgical procedures, can lead to significant respiratory complications, particularly concerning respiratory complications. Three primary causes of such complications are dyskinesia, the loss of sigh breath, and an increase in the fraction of inspired oxygen (FIO2). These factors prominently contribute to the development of compression and absorption atelectasis during anesthesia (1,2). Atelectasis, characterized by the collapse of alveoli, poses a serious threat to respiratory function during and after surgical procedures. The elimination of the sigh reflex, which naturally occurs under general anesthesia, plays a pivotal role in this process. The sigh reflex is a protective mechanism that helps keep the alveoli open by periodically taking deeper breaths. When this reflex is suppressed by anesthesia, atelectasis can develop rapidly, affecting 100% of patients under general anesthesia as documented in numerous studies. This rapid alveolar collapse disrupts normal gas exchange, leading to decreased arterial oxygenation and increased risk of postoperative pulmonary complications (3,4). The impact of atelectasis on patients’ outcomes cannot be overstated. It not only hampers gas exchange, but also predisposes patients to infections and longer recovery times. Therefore, addressing this issue is of paramount importance in anesthetic management. One of the promising approaches to mitigate this problem is the use of alveolar recruitment maneuver (ARM) (5).
ARM aims to reopen collapsed alveoli and to maintain their patency throughout the duration of anesthesia. These techniques involve the application of intermittent positive airway pressure or sustained inflation, which helps re-expand the collapsed alveoli, enhance gas exchange, and subsequently improve arterial oxygenation. The efficacy of these maneuvers is well-documented in the literature. For instance, research has shown that alveolar recruitment maneuvers can significantly reduce the incidence of postoperative pulmonary complications, improve oxygenation, and shorten the length of hospital stays (5-7).
The integration of ARM into mechanical ventilator settings represents a significant advancement in anesthetic practice. Modern mechanical ventilators are equipped with sophisticated settings that allow for the precise application of these maneuvers, tailored to the individual needs of the patient. This integration not only enhances the effectiveness of ventilation, but also simplifies the process for anesthesiologists, ensuring that optimal lung function is maintained throughout the procedure (5,6). In this context, the GE Healthcare Carestation 750 stands out as a state-of-the-art ventilator that incorporates advanced alveolar recruitment techniques. This study aims to evaluate the efficacy of these maneuvers as implemented in Carestation 750. By systematically analyzing its impact on gas exchange, alveolar recruitment and arterial oxygenation, we seek to determine the effectiveness of this technology in clinical practice.
Understanding the mechanics and benefits of these ARMs is crucial for anesthesiologists and healthcare professionals. As the use of general anesthesia continues to rise, the need for effective strategies to prevent and manage atelectasis becomes increasingly critical. The aim of our study was to evaluate the efficacy of different alveolar recruitment maneuvers incorporated in GE Healthcare Carestation 750.
Materials and Methods
Study Design and Setting
This study was conducted at the University Clinic for Anesthesiology, Reanimation and Intensive Care Medicine, Clinical Center “Mother Theresa”, Faculty of Medicine, “Ss. Cyril and Methodius” University, Skopje, Republic of North Macedonia. The study protocol was reviewed and approved by the internal ethical review board of the institution. Informed consent was obtained from all participating patients prior to their inclusion in the study.
Participants
The study included patients aged 18 to 60 years, classified as American Society of Anesthesiologists (ASA) Physical Status I-III, who were scheduled for surgical interventions requiring general endotracheal anesthesia. Exclusion criteria included: pregnant woman, patients with any known history of cardiac or respiratory diseases to minimize confounding variables that could affect pulmonary function and the outcomes of the study.
Anesthesia and Intervention Protocol
After obtaining informed consent, the patients were prepared for surgery according to standard preoperative protocols. General anesthesia was induced using a standardized regimen, and tracheal intubation was performed. Upon successful induction of anesthesia and intubation, patients were randomly assigned to one of three groups:
Group I: Control Group (No Intervention)
Patients in this group received no additional intervention beyond standard ventilation settings.
Group II: Single-Step Recruitment Maneuver
Patients in this group underwent a single-step alveolar recruitment maneuver, which involved applying a sustained inspiratory pressure of 40 cmH2O for 20 seconds.
Group III: Multiple-Step Recruitment Maneuver
Patients in this group underwent a multi-step alveolar recruitment maneuver, which was performed as follows:
Step I: Inspiratory pressure (Pinsp) of 30cmH2O with positive end-expiratory pressure (PEEP) of 10cmH2O for 3 breaths.
Step II: Inspiratory pressure (Pinsp) of 40cmH2O with PEEP of 10cmH2O for 3 breaths.
Step III: Inspiratory pressure (Pinsp) of 50cmH2O with PEEP of 15cmH2O for 3 breaths.
The FiO2 was maintained at 50% for all groups throughout the procedure.
Outcome Measures
The primary outcome measure was the change in pulmonary compliance, which was assessed by measuring compliance before and after the recruitment maneuvers.
Secondary outcome measures included changes in arterial oxygen tension (PaO2) and the PaO2/FIO2 ratio. Arterial blood gas (ABG) analyses were performed at two time-points: before the induction of anesthesia and after the recruitment maneuvers. The ABG samples were analyzed to determine PaO2 levels, which were then used to calculate the PaO2/FIO2 ratio where the FiO2 was maintained at 50% for all groups throughout the procedure.
Data Collection and Analysis
All data were collected by trained anesthesia personnel who were blinded to the group assignments to minimize bias. The collected data included patients’ demographics, baseline pulmonary function and outcome measures (pulmonary compliance, PaO2, and PaO2/FIO2 ratios). Statistical analyses were performed using appropriate statistical software. Continuous variables were expressed as means ± standard deviations, and categorical variables were presented as frequencies and percentages. Differences between groups were analyzed using analysis of variance (ANOVA). A p-value of <0.05 was considered statistically significant.
Figure 1. Recruitment Maneuver Intervention Protocol.
Figure 2. Single step alveolar recruitment maneuver.
Figure 3. Multi step alveolar recruitment maneuver.
Results
A total of 75 patients were enrolled in this study, with 25 patients allocated to each of the three groups (Group I: Control, Group II: Single-Step Recruitment, Group III: Multiple-Step Recruitment). The demographic and baseline characteristics of the patients were comparable across the three groups, with no significant differences in age, gender, body mass index (BMI), or ASA physical status classification.
The primary outcome measure, pulmonary compliance, showed significant improvements in the groups that underwent alveolar recruitment maneuvers. Specifically, Group III (Multiple-Step Recruitment) exhibited a 37% increase in pulmonary compliance compared to baseline values, while Group II (Single-Step Recruitment) demonstrated a 24% increase. In contrast, the control group (Group I) showed no significant change in compliance (Table 1).
Table 1. Respiratory parameters in the Groups.
| Group | Compliance mL/cmH20 | PaO2 mmHg | PaO2/FIO2 | |||
| Baseline | After intervention | Baseline | After intervention | Baseline | After intervention | |
| I | 53 ± 6.8 | / | 97 ± 23 | / | 421 ± 44 | / |
| II | 53 ± 6.7 | 65 ± 7.8 | 146 ± 27 | 177 ± 26 | 481 ± 31 | 584 ± 51 |
| III | 53 ± 5.0 | 72 ± 6.9 | 135 ± 27 | 172 ± 30 | 444 ± 34 | 567 ± 41 |
PaO2 – partial pressure of oxygen; PaO2/FIO2 – the ratio of arterial oxygen partial pressure to fractional inspired oxygen
The data revealed a significant increase in PaO2 levels in both recruitment maneuver groups compared to the control group. The mean PaO2 increased markedly in Group II and Group III, indicating enhanced oxygenation due to the recruitment maneuvers. Statistical analysis confirmed that these increases were significant (P<0.05).
No adverse events or complications were reported during or following the alveolar recruitment maneuvers in any of the groups. All patients tolerated the procedures well, and there were no instances of hemodynamic instability, barotrauma, or other respiratory complications associated to the recruitment maneuvers.
Discussion
These results collectively demonstrate that ARM significantly enhances pulmonary compliance and oxygenation without compromising patients’ safety. The multi-step recruitment approach, in particular showed the most pronounced benefits, suggesting that a gradual and stepped increase in inspiratory pressures may be more effective in recruiting alveoli and improving respiratory mechanics. These results highlight the efficacy of ARM in improving lung mechanics during general anesthesia (6,7). This improvement underscores the effectiveness of ARM in enhancing gas exchange and maintaining adequate oxygenation during surgery. The observed improvements in pulmonary compliance and oxygenation suggest that incorporating ARM into standard anesthetic practice can enhance patients’ outcomes by preventing and reversing atelectasis. Atelectasis, a common complication of general anesthesia, can lead to impaired gas exchange, hypoxemia and increased risk of postoperative pulmonary complications. By effectively recruiting collapsed alveoli, recruitment maneuvers help maintain optimal lung function, thereby reducing the risk of these complications (4,8).
Our findings align with previous studies that have reported the benefits of ARM. For instance, Hedenstierna demonstrated that recruitment maneuvers prevent atelectasis and improve oxygenation during general anesthesia. Similarly, Hartland et al. highlighted the efficacy of various recruitment strategies in enhancing pulmonary function. The consistency between our results and these earlier studies reinforces the robustness of ARM as an effective intervention for improving intraoperative respiratory outcomes (9,10).
In addition to these foundational studies, several other investigations have explored the benefits of ARM. Neumann et coauthors reported that systematic recruitment maneuvers significantly improved gas exchange and reduced the incidence of postoperative pulmonary complications in patients undergoing cardiac surgery (7). Similarly, an article of Fernandez-Bustamante demonstrated that a stepwise recruitment maneuver combined with individualized PEEP titration resulted in improved oxygenation and lung mechanics in patients with acute respiratory distress syndrome (ARDS) undergoing surgery (11). These studies further corroborate our findings and emphasize the utility of ARM across various surgical and clinical contexts. Moreover, in another study, the same authors showed that intraoperative ARM combined with high PEEP levels improved respiratory function and reduced atelectasis in obese patients undergoing laparoscopic surgery (12). Other studies also investigate the ARM in obese patients undergoing laparoscopic surgery and its benefits on respiratory effects after pneumo-peritoneum deterioration (13). Those study highlight the potential benefits of ARM in high-risk patient populations, supporting the broader applicability of our findings (7,11-15).
The study also confirms the safety and feasibility of performing ARM in an intraoperative setting. None of the patients experienced adverse events related to the recruitment procedures, indicating that both single-step and multiple-step maneuvers can be safely integrated into standard anesthetic protocols. This safety profile is critical for the widespread adoption of these techniques, as it reassures clinicians that recruitment maneuvers do not introduce additional risks to patient care (11-15).
The present plethora of literature provides an update on alveolar recruitment approaches taking into account the wide range of variations in their use, as well as the various parameters influencing the response to movement. Recruitment techniques could stop the reduction in oxygenation brought on by mechanical ventilation and lung de-recruitment (5,6,10-15). A panel of experts created consensus recommendations for the surgical patient’s intraoperative protective ventilation. It is important to stress that two research topics fell short of the 70% consensus threshold. First, there is insufficient high-quality supporting evidence to support the routine recommendation of ARM for all patients following tracheal intubation, yet a majority of 57% agreed that it might be taken into consideration based on a unique risk-benefit analysis (16). Hartland and colleagues reviewed the literature and assessed the various alveolar recruitment techniques. With the exception of one study, various ARMs were identified (10). The researchers performed persistent manual inflations up to a PIP of 40cm H2O for their alveolar recruitment procedures. Pang et al. used ten sustained manual inflations over one minute, while Almarakbi et al. used a single sustained inflate for fifteen seconds. In both trials, the groups who underwent ARM had higher intraoperative PaO2. On pulmonary compliance, however, only Almarakbi et al. published findings, which indicated a rise only in the groups that underwent ARM. Airway resistance and PaO2/FIO2 were not discussed in either study contrary to our investigations who take these variables into account (17,18). Three studies used stepwise PEEP increases as an ARM, beginning at 4cm H2O and ending at 20cm H2O. There was a statistically significant increase in the groups that underwent ARM in both studies that included intraoperative PaO2. The pulmonary compliance of the ARM groups improved in all three trials. Findings were confirmed in our study as well. PaO2/FIO2 was only used as an outcome measure by Springer et al. and Whalen et al., and it was considerably higher in the ARM groups during the intraoperative phase (19,20).
Future research should also explore the long-term benefits of ARM, including their impact on postoperative recovery, length of hospital stay and overall patients’ morbidity and mortality. Additionally, investigating the mechanistic aspects of recruitment maneuvers, such as their effects on lung tissue and inflammatory responses, could provide deeper insights into their therapeutic benefits. Comparative studies evaluating different recruitment strategies and their outcomes in various surgical and clinical contexts would also be valuable.
Conclusion
In conclusion, our study validates that in patients receiving general endotracheal anesthesia, alveolar recruitment maneuvers considerably improve arterial oxygenation and pulmonary compliance. To enhance patients’ safety and respiratory outcomes, these methods ought to be included into routine anesthetic practice.
References:
- Brismar B, Hedenstierna G, Lundquist H, Strandberg A, Svensson L, Tokics L. Pulmonary densities during anesthesia with muscular relaxation–a proposal of atelectasis. Anesthesiology. 1985 Apr;62(4):422-8. doi: 10.1097/00000542-198504000-00009.
- Ruscic, Katarina J.a; Grabitz, Stephanie D.a; Rudolph, Maíra I.a; Eikermann, Matthiasa,b. Prevention of respiratory complications of the surgical patient: actionable plan for continued process improvement. Current Opinion in Anaesthesiology, 2017;30(3): p 399-408.
- Fan J, Ye RD, Malik AB. Transcriptional mechanisms of acute lung injury. Am J Physiol Lung Cell Mol Physiol. 2001; 281:L1037–50.
- Magnusson L, Spahn DR. New concepts of atelectasis during general anaesthesia. Br J Anaesth. 2003 Jul;91(1):61-72. doi: 10.1093/bja/aeg085. PMID: 12821566.
- Chacko J, Rani U. Alveolar recruitment maneuvers in acute lung injury/acute respiratory distress syndrome. Indian J Crit Care Med. 2009 Jan-Mar;13(1):1-6. doi: 10.4103/0972-5229.53107. PMID: 19881171; PMCID: PMC2772255.
- Lachmann B. Open up the lung and keep the lung open. Intensive Care Med. 1992;18(6):319-21. doi: 10.1007/BF01694358. PMID: 1469157.
- Neumann, P., et al. “Atelectasis and Alveolar Recruitment.” Critical Care, vol. 6, no. 4, 2002, pp. 344-350.
- Bendixen, H. H., et al. “Impaired Oxygenation in Surgical Patients during General Anesthesia with Controlled Ventilation.” The New England Journal of Medicine, vol. 269, 1963, pp. 991-996.
- Hedenstierna, G. Atelectasis during anesthesia: Can it be prevented?. J Anesth 11, 219–224 (1997). https://doi.org/10.1007/BF0248004.
- Hartland BL, Newell TJ, Damico N. Alveolar recruitment maneuvers under general anesthesia: a systematic review of the literature. Respir Care. 2015 Apr;60(4):609-20. doi: 10.4187/respcare.03488. Epub 2014 Nov 25.
- Fernandez-Bustamante A, Sprung J, Parker RA, Bartels K, Weingarten TN, Kosour C, Thompson BT, Vidal Melo MF. Individualized PEEP to optimise respiratory mechanics during abdominal surgery: a pilot randomised controlled trial. Br J Anaesth. 2020 Sep;125(3):383-392. doi: 10.1016/j.bja.2020.06.030.
- Fernandez-Bustamante A, Sprung J. Intraoperative Positive End-expiratory Pressure for Obese Patients: A Step Forward, a Long Road Still Ahead. Anesthesiology. 2021 Jun 1;134(6):838-840. doi: 10.1097/ALN.0000000000003806.
- Futier E, Constantin JM, Pelosi P, Chanques G, Kwiatkoskwi F, Jaber S, Bazin JE. Intraoperative recruitment maneuver reverses detrimental pneumoperitoneum-induced respiratory effects in healthy weight and obese patients undergoing laparoscopy. Anesthesiology. 2010 Dec;113(6):1310-9. doi: 10.1097/ALN.0b013e3181fc640a.
- Hemmes SN, Gama de Abreu M, Pelosi P, Schultz MJ. High versus low positive end-expiratory pressure during general anaesthesia for open abdominal surgery (PROVHILO trial): a multicentre randomised controlled trial. Lancet. 2014 Aug 9;384(9942):495-503. doi: 10.1016/S0140-6736(14)60416-5. Epub 2014 Jun 2.
- Gonçalves LO, Cicarelli DD. Alveolar recruitment maneuver in anesthetic practice: how, when and why it may be useful. Rev Bras Anestesiol. 2005 Dec;55(6):631-8. English, Portuguese. doi: 10.1590/s0034-70942005000600006.
- Young C, Harris E, Vacchiano C et al. Lung-protective ventilation for the surgical patient: international expert panel-based consensus recommendations. British Journal of Anaesthesia 2019; 123,(6): 898e913. doi: 10.1016/j.bja.2019.08.017.
- Almarakbi WA, Fawzi HM, Alhashemi JA. Effects of four intraoperative ventilatory strategies on respiratory compliance and gas exchange during laparoscopic gastric banding in obese subjects. Br J Anaesth 2009;102(6):862-868.
- Pang CK, Yap J, Chen PP. The effect of an alveolar recruitment strategy on oxygenation during laparoscopic cholecystectomy. Anaesth Intensive Care 2003;31(2):176-180.
- Sprung J, Whalen FX, Comfere T, et al. Alveolar recruitment and arterial desflurane concentration during bariatric surgery. Anesth Anal 2009;108(1):120-127.
- Whalen FX, Gajic O, Thompson GB, et al. The effects of the alveolar recruitment maneuver and positive end-expiratory pressure on arterial oxygenation during laparoscopic bariatric surgery. Anesth Analg 2006;102(1):298-305.