UDK: 616-089.5-032:611.819.59]:616-089.168
https://www.doi.org/10.55302/MJA2484086ch
Chavkoska M1, Shosholcheva M2, Zimoska A3, Naumovski F3, Gavrilovska Brzanov A3
1General Hospital of Ohrid, Department of Anesthesiology and Intensive Care Medicine,
2University Clinic for Traumatology, Orthopedics, Anesthesiology, Resuscitation, Intensive Care and Emergency Center – Skopje, Department of Anesthesiology, Resuscitation and Intensive Care Medicine, “Ss. Cyril and Methodius” University – Skopje, Faculty of Medicine
3University Clinic of Surgical Diseases “St. Naum Ohridski” Skopje, Republic of North Macedonia
Abstract
Introduction: Epidural anesthesia is particularly suitable for patients in older age brackets. While it was previously the predominant approach for postoperative analgesia across various procedures, alternative methods that are equally effective, potentially safer, and more cost-efficient have since emerged. This article will explore the advantages and drawbacks of continuous epidural analgesia intraoperatively, particularly its outcomes in specific surgical contexts.
Material and methods: The University Clinic for Traumatology, Orthopedics, Anesthesiology, Resuscitation, Intensive Care and Emergency Center, enrolled twenty patients in an observational clinical study over a six-months period to assess the comprehensive management of analgesia during the intraoperative and postoperative phases. After induction of GA, Bupivacaine 0.125% was administered by a continuous epidural infusion until the end of the surgery. Postoperative outcomes included assessing pain levels immediately after surgery, 3, 6, 12 and 24 hours later, as well as the incidence of postoperative complications, if any.
Results: The study enrolled twenty patients who underwent a combination of general anesthesia and epidural anesthesia. We measured the patients’ postoperative pain, and the results showed that the most pain typically flares up three hours after surgery and then subsides over the next 24 hours. On the first day following surgery, the average VAS was 1.8. Postoperative nausea and vomiting occurred in every patient who had morphine administered as postoperative analgesia.
Conclusion: The study concludes that continuous epidural analgesia reduces the need for opioid use and mitigates the associated side effects.
Keywords: epidural analgesia; postoperative nausea and vomiting; visual analogue scale.
Introduction
Continuous epidural analgesia can be employed for managing postoperative pain following thoracic, abdominal or lower extremity surgery. While it was previously widely adopted as the standard approach for postoperative pain relief across various procedures, alternative methods that are equally effective, potentially safer and more cost-efficient, have now become available (1). Continuous epidural analgesia is predominantly utilized in open surgeries, although it can also be employed in genitourinary or lower extremity procedures. Epidural catheters are typically reserved for patients expected to remain hospitalized for more than 24 hours post-surgery and are seldom utilized in minimally invasive procedures. Over time, the indications for and utilization of continuous epidural analgesia have diminished due to shorter hospital stays for many surgeries, increased adoption of minimally invasive techniques, and advancements in perioperative pain management strategies. Multimodal approaches focusing on sparing opioids with nonopioid analgesics, peripheral nerve blocks, local anesthetic infiltration and other methods, have emerged as viable alternatives. These strategies can provide equivalent pain relief to epidural analgesia for many procedures while mitigating the risks, side effects and costs associated with epidurals. Epidural analgesia remains part of some enhanced recovery after surgery protocols, sometimes offered alongside other regional anesthesia options as alternatives. Furthermore, epidural techniques are increasingly employed for diagnostic procedures, acute pain management and the treatment of chronic pain. Epidural blocks have been demonstrated to potentially decrease the surgical stress response, lower the risk of cancer recurrence, reduce the incidence of perioperative thromboembolic events, and potentially lower the morbidity and mortality related to major surgery (2,3). Neuraxial anesthesia, when compared to general anesthesia, offers several potential advantages. These include reduced intraoperative blood loss and transfusion requirements, a lower incidence of postoperative thromboembolic events, improved pain relief and postoperative mobility up to 9 weeks after surgery, quicker return of bowel function, and other debated benefits such as shorter hospital stays and reduced healthcare costs (4). During open surgeries, patients may require significant sedation if not undergoing a combined general-neuraxial approach. A sensory level typically around T6 is necessary, with catheter placement usually in the midthoracic region (5). The aim of this study was to evaluate the impact of continuous epidural analgesia on reducing the necessity for opioid use, mitigating their associated side effects, and improving overall patients’ outcomes in the postoperative period. Additionally, to assess the benefits of this analgesic approach in enhancing patient’s comfort, satisfaction, and recovery in comparison to traditional opioid-based pain management strategies.
Material and Methods
Top of Form
Bottom of Form
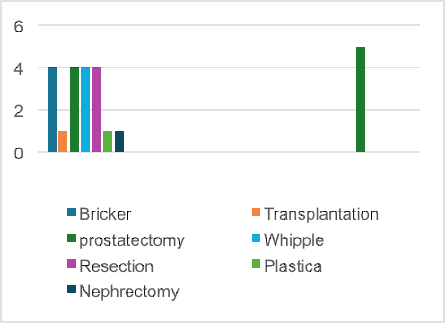
Since January 1, 2024, at the University Clinic for Traumatology, Orthopedics, Anesthesiology, Resuscitation, Intensive Care and Emergency Center – Skopje, a prospective database was maintained for patients undergoing radical cystectomy (RC), kidney transplantation, prostatectomy, Whipple surgery and nephrectomy (Chart 1). Approval from the Internal Hospital Ethics Committee and written informed consent from patients were secured prior commencing the study. The American Society of Anesthesiologists (ASA) score was evaluated for all patients and all of them abstained from eating or drinking after midnight on the night before surgery. Standard hemodynamic monitoring (including electrocardiogram, pulse oximetry and non-invasive blood pressure measurement) was performed before anesthesia induction. An epidural catheter was administered before anesthesia induction. The patients receiving epidural, were positioned sitting up, and the L1-L2 epidural space was located using an 18G Touhy needle with a loss of resistance technique. Subsequently, placement of the epidural catheter was confirmed by a negative aspiration test using 2ml of 0.5% bupivacaine. All patients were induced to general anesthesia, adequately with benzodiazepines, midazolam (0.02-0.04mg/kg), propofol (1.5-2.5mg/kg), rocuronium bromide (0.6-1mg/kg) and Fentanyl in range of 0 to 20mcg before laryngoscopy and intubation. After the induction of general anesthesia, it was maintained with Sevoflurane (1/2%), and Bupivacaine 0.125% was administered by a continuous epidural infusion until the end of the operation.
Postoperative pain management relied on NSAIDs (non-steroidal anti-inflammatory drugs), Acetaminophen, Methimazole, based on sufficient measurement of pain intensity, according to VAS scale (The Visual Analogue Scale (VAS) measures pain intensity). The VAS consists of a 10cm line, with two end points representing 0 (‘no pain’) and 10 (‘pain as bad as it could possibly be’). Postoperative outcomes included assessing pain levels immediately after surgery, 3, 6, 12 and 24 hours later, as well as the percentage of complications if any occurred.
All data were gathered by trained anesthesia staff who were not involved in patients’ care to reduce bias. Patients’ demographics, perioperative data and outcome metrics were among the information gathered. Statistical software was used to carry out statistical analyses. Categorical variables were displayed as frequencies and percentages, whereas continuous variables were given as means ± standard deviations.
Results
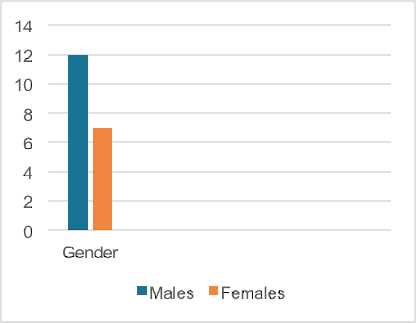
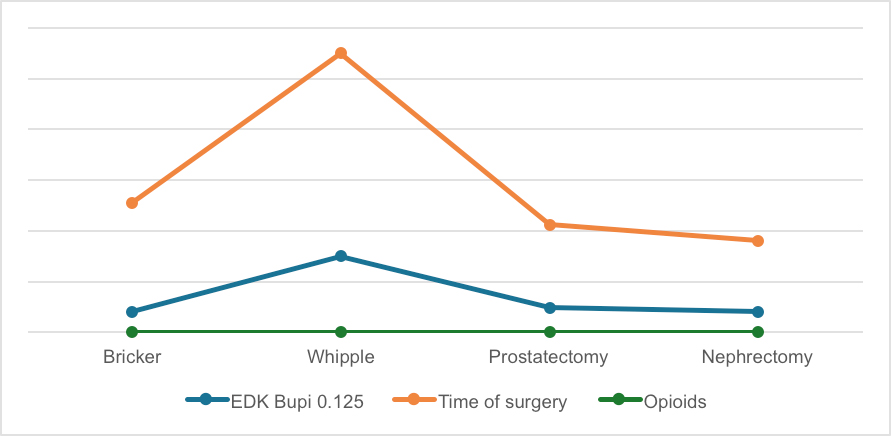
In this evaluation, 20 patients were recruited who were operated under combined general anesthesia and epidural anesthesia. Thirteen of the patients were males, seven females (Chart 2) and the age range of the group was between 37 and 79 years, with average age of 64.15 years. The body mass index varied between 21 and 32, an average of 26.15. Total administration of Bupivacaine 0.125% was in range of 20ml for Bricker surgery in duration of 200 minutes, to 150ml for Whipple in duration of 550 minutes (Chart 3).
Chart 1. Types of surgeries. Chart 2. Gender of patients.
Chart 3. Average use of Bupivacaine 0.125%, use of Opioids and duration of surgery.
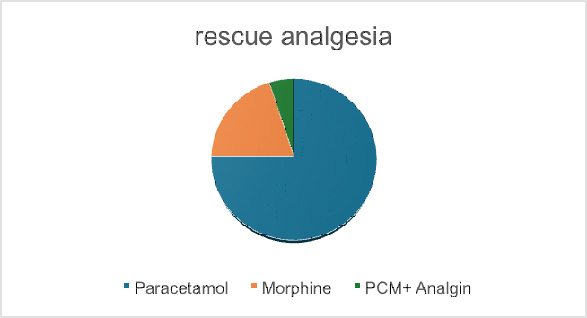
After reviewing the data, it was found that patients who received continuous epidural analgesia, with dosage adjusted based on surgery length and patients’ needs, required less opioid pain relief. The patients with a greater body mass index (BMI) necessitated higher amount of pain relief medication. Postoperative outcomes included assessing pain levels immediately after surgery, 3, 6, 12 and 24 hours after surgery, and the incidence of postoperative nausea and vomiting. The patients experienced peak pain intensity 3 hours after surgery, with pain levels gradually decreasing over the next 24 hours. After surgery, the majority of patients relied on acetaminophen and methimazole for postoperative pain relief (Chart 4). Four out of twenty patients have a demand for postoperative analgesia with Morphine (2-3mg), according to VAS. Subsequently, all experienced postoperative nausea and vomiting.
Discussion
The International Association for the Study of Pain (IASP) defines pain as an unpleasant emotional and sensory experience that is either described, or actually connected to potential tissue damage (5). The opioid system is a vital physiological mechanism that regulates pain, emotions, immune responses and various other bodily functions. It encompasses the interaction and coordination of numerous endogenous opioid peptides and various types of opioid receptors located in both the central nervous system (CNS) and peripheral nervous system (6).
Opioids are commonly prescribed to treat moderate to severe acute and chronic pain. However, these medications have significant drawbacks, such as inducing tolerance to pain relief, addiction, and various behavioral side effects that frequently lead to patient’s non-adherence (7). All opioids used in clinical practice act as agonists on the μ-opioid receptor, and the main adverse effects are either directly related to this receptor or potentially influenced by its activation. While opioids are highly effective in managing pain, it is crucial to acknowledge their associated side effects as well. Side effects are prevalent with opioid therapy, with between 50% and 80% of patients in clinical trials experiencing at least one side effect. In real-world usage, the incidence of side effects may be even higher (1). Respiratory depression is a significant concern linked to the use of opioids, particularly in acute pain management when patients have not yet developed tolerance. In cases of persistent pain, the risk is more likely to arise if there is a substantial, often unintended increase in dosage, or changes in the formulation or method of administration. Tolerance, which involves a diminishing response to opioids’ pain-relieving effects, is a frequent complication of opioid therapy. This often results in the need for higher doses of opioids to achieve the same level of pain relief, ultimately reducing their effectiveness over time. The impact of opioid compounds on hormonal function is now well-documented and referred to as opioid endocrinopathy (OE) or opioid-induced androgen deficiency (OPIAD) in the case of androgen hormones. These hormonal effects occur in both men and women and have been observed with oral consumption, transdermal, intravenous and intrathecal administration of opioids. Hyperalgesia, also known as hypalgia, is a recently recognized adverse effect characterized by heightened pain sensitivity. This phenomenon manifests as escalating pain levels despite increasing doses of opioids. Prolonged and high-dose opioid use may lead to the development of hyperalgesia, potentially influenced by opioid metabolites like morphine 3-glucuronide (M3G). The most common side effects of opioid usage are constipation (which has a very high incidence) and nausea. Constipation is a prevalent issue, affecting 40% to 95% of patients receiving opioid treatment, and can occur even after a single dose of morphine. The mechanisms underlying opioid-induced nausea and vomiting (OINV) are not completely understood, but they likely involve multiple complex factors. OINV may result from various opioid effects, including heightened sensitivity in the vestibular system (manifesting as symptoms like vertigo exacerbated by motion), direct actions on the chemoreceptor trigger zone, and delayed gastric emptying (leading to symptoms such as early satiety, bloating and worsening after meals). The side effects of opioid are sedation, dizziness, delayed gastric emptying, muscle rigidity, pruritus and dry mouth (8-14).
On the other hand, we have to mention side effects of placing an epidural catheter, which are typically transient. Decreased blood pressure, leading to feelings of dizziness or nausea, temporary urinary incontinence, pruritus (itchy skin), nausea, headaches and nerve injury are some of them, as documented in existing literature (2). It is evident that there is some similarity in the side effects of opioids and epidural anesthesia, which largely depends on the medications administered via the epidural catheter (2,15). The primary aim of this study was to mitigate these side effects by continuously delivering bupivacaine as a local anesthetic through the catheter. Considering both absolute contraindications (such as patients’ refusal, sepsis and hypersensitivity to potential medications) and relative contraindications (including infection, coagulation disorders, prior spinal surgery, neurological conditions, thrombocytopenia and coagulopathies), we can mitigate risks to patients’ health while maximizing the benefits of continuous epidural analgesia.
Conclusion
Continuous epidural analgesia intraoperatively effectively reduces the need for opioid medications and their associated side effects. Despite the proven effectiveness of opioids in treating various pain conditions, their use can result in significant side effects and complications. The study’s evaluations highlight that epidural analgesia provides a viable alternative, minimizing the reliance on opioids and mitigating their negative impacts.
References:
- Inge Tamm-Daniels, MD, Shelby Badani, MD, MSPH, MS, Melanie Donnelly, MD, MPH, MBA, Continuous epidural analgesia for postoperative pain: Benefits, adverse effects, and outcomes. In: UpToDate, Connor RF (Ed), Wolters Kluwer. (Accessed on June 17, 2024.).
- Chou R, Gordon DB, de Leon-Casasola OA, Rosenberg JM, et al. Management of Postoperative Pain: A Clinical Practice Guideline From the American Pain Society, the American Society of Regional Anesthesia and Pain Medicine, and the American Society of Anesthesiologists’ Committee on Regional Anesthesia, Executive Committee, and Administrative Council. J Pain. 2016 Feb;17(2):131-57.
- Rawal N. Epidural analgesia for postoperative pain: Improving outcomes or adding risks? Best Pract Res Clin Anaesthesiol. 2021 May;35(1):53-65.
- Teng IC, Sun CK, Ho CN, Wang LK, Lin YT, Chang YJ, Chen JY, Chu CC, Hsing CH, Hung KC. Impact of combined epidural anaesthesia/analgesia on postoperative cognitive impairment in patients receiving general anaesthesia: a meta-analysis of randomised controlled studies. Anaesth Crit Care Pain Med. 2022 Oct;41(5):101119.
- Hadzic A. eds. NYSORA Textbook of Regional Anesthesia and Acute Pain Management. The McGraw-Hill Companies; 2007. Accessed June 17, 2024. https://accessanesthesiology.mhmedical.com/content.aspx?bookid=413§ionid=39828140.
- State Insurance Regulatory Authority: Guidelines for the management of acute whiplash-associated disorders – for health professionals. Sydney: third edition, 2014.
- Raja SN, Carr DB, Cohen M, et al. The revised International Association for the Study of Pain definition of pain: concepts, challenges, and compromises. Pain. 2020;161(9):1976-1982.
- Cai Z, Ratka A. Opioid system and Alzheimer’s disease. Neuromolecular Med. 2012;14(2):91-111.
- Walsh, T. Declan. “Common misunderstandings about the use of morphine for chronic pain in advanced cancer.” CA: A Cancer Journal for Clinicians 35, no. 3 (1985): 164-169.
- Melzack R. From the gate to the neuromatrix. Pain. 1999; Suppl 6:S121-S126.
- Holden JE, Jeong Y, Forrest JM. The endogenous opioid system and clinical pain management. AACN Clin Issues. 2005;16(3):291-301.
- Paul AK, Smith CM, Rahmatullah M, et al. Opioid Analgesia and Opioid-Induced Adverse Effects: A Review. Pharmaceuticals (Basel). 2021;14(11):1091. Published 2021 Oct 27.
- Benyamin R, Trescot AM, Datta S, et al. Opioid complications and side effects. Pain Physician. 2008;11(2 Suppl): S105-S120.
- Smith, H., Smith, J., & Seidner, P. (2012). Opioid-induced nausea and vomiting. Annals Of Palliative Medicine, 1(2), 121-129.
- Naji P, Farschtschian M, Wilder-Smith OH, WilderSmith CH. Epidural droperidol and morphine for postoperative pain. Anesth Analg 1990; 70:583-588.