UDK: 616.31-051-057:[616.98:579.828.7(497.7)“2023“
Petresкa1, S. Kondova2, M. Stevanoviкј1, A. Atanasovska-Stojanovska2,3, V. Saveski1, S. Spasovski4.
1PHO University Clinic for Infectious Diseases and Febrile Conditions, Skopje, “Ss. Cyril and Methodius” University Skopje, Faculty of Medicine – Skopje
2PHO University Dental Clinical Center “Saint Panteleimon”, Skopje, Clinic for Oral and Periodontal Diseases
3“Ss. Cyril and Methodius” University Skopje, Faculty of Dentistry – Skopje, Department of Oral and Periodontal Diseases
4“Ss. Cyril and Methodius” University Skopje, Faculty of Dentistry – Skopje, Department of Oral Surgery
Abstract
The transmission of blood-borne diseases, such as HIV infection, hepatitis B and hepatitis C virus infection, still represents a risk for professional exposure among healthcare workers today.
We present the case of a 39-years-old female patient, first diagnosed with HIV infection in November 2021. As a result of antiretroviral therapy efficiency, undetectable values of HIV RNA viral load in serum and immune reconstitution were achieved.
In December 2023, the patient was presented to the University Dental Clinical Center due to tooth pain for a dental examination. A diagnosis of chronic apical periodontitis of the tooth (VI lower right) was made, after which the patient was advised to continue treatment at the Clinic of Oral and Periodontal Diseases. After the examination, presence of dental plaque cleaning was done, and a drain was placed in the periodontal pocket after curettage. During the examination and dental interventions, the medical staff used standard protective equipment, protective gloves, a mask and protective glasses. Examination and treatment procedures were carried out in compliance with the appropriate protocols of evidence-based medicine, and the correct disposition of the used medical material was made.
Key Words: HIV infection, chronic apical periodontitis, professional exposure.
INTRODUCTION
The transmission of blood-borne diseases, such as HIV infection, hepatitis B and hepatitis C virus infection, still represents a risk for professional exposure among healthcare workers today. Based on data from the World Health Organization (WHO), it is estimated that approximately 2.5% of HIV infections, 40% of hepatitis B and hepatitis C virus infections among health workers are the result of professional exposure (1).
HIV infection is transmitted through direct contact with body fluids containing the HIV virus from an HIV-infected person, as blood, breast milk, seminal fluid and vaginal secretions. Also, HIV can be transmitted by vertical transmission from mother to child during pregnancy and childbirth (2).
Professional exposure to HIV infection in healthcare workers is the most often through percutaneous injuries involving needlesticks or cuts from sharp objects, contact with mucous membranes or skin (especially if the skin is damaged due to injuries or dermatitis, or if the contact is prolonged or larger areas of skin surfaces are affected), with HIV-infected body fluids. Many factors influence the risk of professional transmission of HIV infection, such as the use of personal protective equipment, the type of injury, the prevalence of HIV infection in the country, the frequency and number of exposures, and of course the level of HIV RNA viral load at the source of HIV infection (3). It is important to note that persons with HIV infection who regularly receive antiretroviral therapy (ART) and have undetectable values of HIV RNA viral load in serum determined by polymerase chain reaction (PCR-polymerase chain reaction), cannot transmit the virus to their sexual partners (2). According to the data from the Centers for diseases control and prevention (CDC) the risk of professional transmission of HIV varies by the type of exposure and it is almost equal to zero in the case of splashing body fluids containing the HIV virus even in cases where there is presence of blood, extremely low in cases of splashing of HIV-infected body fluids on intact skin or mucous membranes and less than 1% in case of percutaneous injuries (needle stick).(4).
The estimated risk of transmission of HIV infection from percutaneous exposure to HIV-infected blood is approximately 0.3%, from exposure to mucous membranes approximately 0.09%, and the risk from eye, nose or mouth exposure to HIV-infected blood is estimated to be approximately 0.1% (1 in 1000) (1).
Dentists play an important role in ensuring the oral health of patients with HIV infection. More than 40 types of oral manifestations are present as clinical manifestations in people with HIV infection, and between 70 and 90% of people living with HIV will have at least one oral manifestation of the disease during their lifetime. Therefore, people with HIV infection need dental care (5).
Some oral manifestations of HIV infection have important diagnostic significance and show the progression of the disease, some cause pain and discomfort, and sometimes they can be life-threatening. The available information is that the risk of transmission of HIV infection in dental offices is very low. The risk of transmission of HIV infection during dental interventions for health professionals is low, due to the fact that saliva does not contain the HIV virus unless it is contaminated with blood (5).
In dentistry, accidental contact with blood occurs when closing syringe needles, during surgical interventions, biopsies, sutures, when disposing of used needles in containers or during transportation of medical waste (1). The specific nature of interventions in dental health care requires the existence of specific strategies and protocols in order to prevent the transmission of HIV infection at dental offices (5).
Prevention of occupational exposure to HIV according to CDC recommendations, is the application of standard protective measures at all times during work with patients, assuming that all blood and body fluids are potentially infected. It is also recommended to use protective gloves, protective glasses, masks and clothing when in contact with body fluids or blood, wash hands and other skin surfaces immediately after contact with blood or body fluids, careful handling and disposal of sharp objects during and after the interventions, use of safe equipment for the prevention of needlesticks, correct disposition of medical waste and sharp objects in containers, reporting the exposure to an appropriate medical person, application of post-exposure prophylaxis (PEP) after an assessment by the medical person (4).
Today, the highly effective ART used in the treatment of HIV infection enables the suppression of viral replication and the drop of the viral load in HIV-infected persons to undetectable values, so that at the same time these persons cannot transmit the infection. WHO recommends the use of ART as PEP in order to prevent the occurrence of HIV infection during professional exposure (2). HIV PEP reduces the possibility of transmission of HIV infection if given within a maximum period of 72 hours after exposure to HIV. The earlier HIV PEP is started, it is better, every hour after exposure is important and counts (4).
In June 2021, in the Republic of North Macedonia an instruction for the application of PEP after professional exposure to HIV was adopted (6). Through the presentation of this case, the importance of informing health personnel about the existence of preventive measures in case of risk exposure to body fluids from an HIV-infected person will be emphasized, which will contribute to reducing the possibility of transmission of HIV infection among health workers, as well as reducing discrimination and stigma for working with people living with HIV.
Case Ppresentation
We present a patient aged 39 years, female, single, smoker, one pack of cigarettes per day, employed in the food industry, first diagnosed with HIV infection in November 2021.
According to the epidemiological data obtained from the history of the disease, the transmission of HIV infection occurred through heterosexual way. The patient was tested for HIV infection at the Institute for Transfusion Medicine in Skopje, when donating blood according to the rules for criteria and procedures for assessment and testing of blood or blood component donors, in accordance with the principles of good transfusion practice published in the official paper in 2009. As part of the blood testing protocol for voluntary blood donors, in addition to testing for blood group and Rh factor, tests for antibody detection, testing for syphilis, testing for hepatitis B and C, the presence of antibodies to the cause of the syndrome was also tested of acquired immunodeficiency (AIDS)-HIV virus. After receiving a positive result for HIV antibodies, the patient was referred to the PHO University Clinic for Infectious Diseases and Febrile Conditions in Skopje as a reference institution, in order to confirm the diagnosis of HIV infection. At the clinic, confirmatory tests of the fourth generation Enzyme linked immunoassay (ELISA) were performed for the detection of antibodies to HIV and p24 antigen, as well as the detection of antibodies by Western blot. The combination of these two tests to confirm the diagnosis of HIV infection has an accuracy of 99.9% (7). The patient was without subjective symptoms and has no history of other past diseases.
After confirming the patient’s HIV infection, a procedure of investigations was started, which included a set of laboratory biochemical and serological investigations, screening for tuberculosis and determination of the degree of immunodeficiency caused by the HIV virus according to the recommendations of the European AIDS Clinical Society (EACS) in order to start ART treatment as soon as possible (Table 1).
Table 1. Laboratory biochemical investigations
| parameter | 25.11.2021 | 28.12.2021 | 03.08.2022 | 08.03.2023 | 04.12.2023 |
| Total bilirubin | 6 | 4 | 6 | 4 | 4 |
| Dir./ind. bilirubin | 2/4 | 1/3 | 2/4 | 1/3 | 1/3 |
| ALT | 20 | 11 | 18 | 26 | 31 |
| AST | 22 | 17 | 19 | 31 | 24 |
| Gama-GT | 30 | 32 | 36 | 83 | 74 |
| glycemia | 5.7 | 5.5 | 5.3 | 6.4 | 5.7 |
| Urea | 4.0 | 2.6 | 2.9 | 2.7 | 2.4 |
| creatinine | 45 | 55 | 55 | 54 | 50 |
| cholesterol | 4.0 | 4.19 | 4.3 | 4.5 | 4.9 |
| triglycerides | 0.67 | 0.8 | 1.15 | 1.42 | 0.98 |
| HDL cholesterol | 1.4 | 1.5 | |||
| LDL cholesterol | 2.46 | 2.9 | |||
| Hgb | 144 | 145 | 153 | 145 | 159 |
| Er | 5190 | 5200 | 5020 | 4740 | 5.20 |
| Le | 4.1 | 3.9 | 4.8 | 4.7 | 6.0 |
| Tr | 271 | 234 | 277 | 243 | 268 |
Serological tests performed during the initial screening of the patient were: HBsAg negative, anti HBc tot negative, anti HBs negative, anti HCV negative, anti-Treponema pallidum IgM and IgG negative, anti -oxoplasma IgM negative, anti EBV IgM negative IgG positive, anti-Cytomegalovirus IgM negative IgG positive.
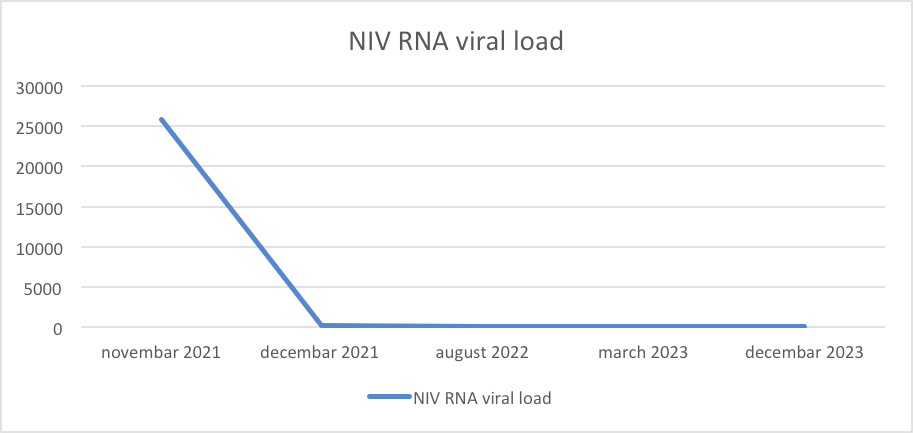
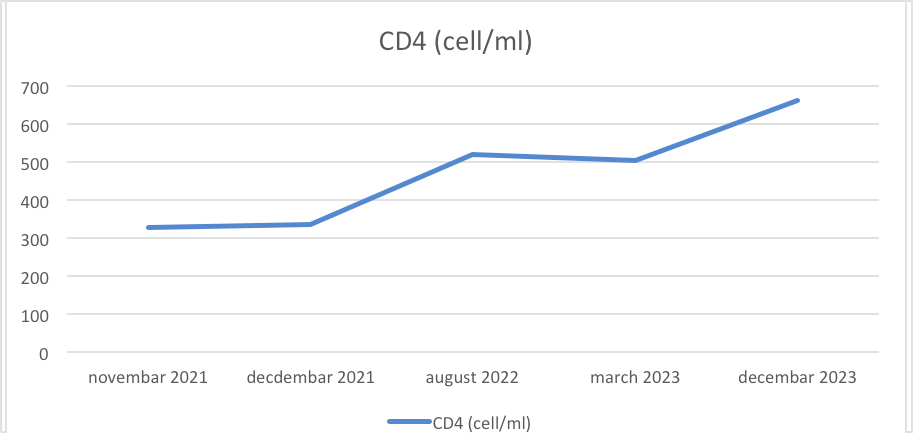
According to the EACS recommendations for the treatment of patients with HIV infection, the patient’s initial combined ART included two nucleoside reverse transcriptase inhibitors (NRTI) – Tenofovir disoproxil/ Emtricitabine and one non-nucleoside reverse transcriptase inhibitor (NNRTI) – Efavirenz. As a result of ART efficiency, undetectable values of HIV RNA viral load in serum and immune reconstitution were achieved (Figure 1) (Figure 2).
Figure 1. Presentation of reduction of HIV RNA viral load in human plasma.
Figure 2. Presentation of immune reconstitution and increase in CD4 cell count.
The quantification of HIV RNA in human plasma was performed using real time polymerase chain reaction RT-PCR Abbot System m2000sp/m2000rt with a lower limit of detection <40 cop/ml, while the determination of immune deficiency using absolute photo-microscopy and light absorption detection on a multicolor platform (Facs Presto-BD) for absolute and percentage detection of CD4 lymphocytes, expressed in the number of cells per milliliter (cell/ml).
In December 2023, the patient was presented to the University Dental Clinical Center due to tooth pain for a dental examination. A diagnosis of chronic apical periodontitis of the tooth (VI lower right) was made, after which the patient was advised to continue treatment at the Clinic of Oral and Periodontal Diseases. After the examination, presence of dental plaque cleaning was done, and a drain was placed in the periodontal pocket after curettage. During the examination and dental interventions, the medical staff used standard protective equipment, protective gloves, a mask and protective glasses. Examination and treatment procedures were carried out in compliance with the appropriate protocols of evidence-based medicine and the correct disposition of the used medical material was made.
After the medical procedures, a consultation was done with an appropriate medical doctor/ person at the Department for HIV infections at the PHO University Clinic for Infectious Diseases and Febrile Conditions to assess the risk of professional exposure and the need for additional preventive measures. An assessment of the risk of transmission of HIV infection was made, taking into consideration all risk factors, including the patient’s current HIV status, and no additional preventive measures were taken.
Discussion
The effectiveness of ART allows the life expectancy of people living with HIV infection to be extended, which in the next period will result in a greater number of patients with HIV infection who will need dental care. Also, certain oral diseases are a frequent clinical manifestation in certain stages of HIV infection, which increases the need for dental interventions and treatment. Therefore, it is necessary to have awareness and knowledge of the risks of professional exposure and transmission of HIV infection when performing dental procedures (8).
A study in Ethiopia showed that professional exposure to HIV infection and the risk of transmission have a significant association with the education and awareness of the health personnel (3). The role of educational training for the prevention of infection transmission is an effective strategy for acquiring skills with which health workers can protect themselves and their colleagues (3).
When assessing the risk of professional exposure to HIV infection in the patient, several risk factors were taken into consideration. One of them was an assessment of the source of HIV infection, where it was established that the patient received ART regularly and had undetectable HIV RNA viral load values in human plasma. The risk of transmission of HIV infection in such cases is extremely low, because the presence of the virus in the blood is not detected, it is present in small amounts in the form of latent infection in certain cell reservoirs (4).
During the dental interventions, the standard measures for protection against professional exposure to HIV infection were applied in accordance with the guidelines for the application of PEP against the transmission of HIV infection from the Ministry of Health of the Republic of North Macedonia (6). The correct disposition of the infectious material was implemented and no exposure to body fluids containing the HIV virus during patient care has been reported. Based on the estimated risk, the need for additional preventive measures such as the use of PEP among health workers was not indicated (6).
Application of HIV PEP shortly after exposure has been shown to reduce the risk of developing HIV infection by 81%. A study in Ethiopia found that 81.6% of exposed health workers did not use HIV PEP. Another study in Kenya also found that less than 45% of health workers did not request HIV PEP due to lack of information, while a study in Cameroon showed nurses’ lack of knowledge about HIV PEP in 73.7% (8). In a study conducted in Cameroon of 312 participants, 63.5% had a professional injury, 51% had adequate knowledge of the existence of HIV PEP recommendations, while 30.3% used HIV PEP (8).
Conclusion
The implementation of standard protection measures, the effectiveness of ART in preventing the transmission of HIV infection, the possibility of applying PEP as prevention in case of professional exposure significantly reduce the risk of transmission of HIV infection. Education of health workers about the risks of transmission during professional exposure to HIV infection will improve the reduction of discrimination and stigma of people who are living with HIV when providing appropriate medical care.
References
- Utkarsha Lokesh, Srinidhi D, Sudhakara Reddy K. Post exposure prophylaxis to occupational injuries for general dentist. J Indian Prosthodont Soc. 2014 Dec;14(Suppl 1):1-3. doi: 10.1007/s13191-012-0176-z. Epub 2012 Oct 5. PMID: 26199484; PMCID: PMC4501978.
- HIV and AIDS, World Health Organization 2024.
- Tsega D, Gintamo B, Mekuria ZN, Demissie NG, Gizaw Z. Occupational exposure to HIV and utilization of post-exposure prophylaxis among healthcare workers at St. Peter’s specialized hospital in Addis Ababa, Ethiopia. Sci Rep. 2023 Apr 29;13(1):7021. doi: 10.1038/s41598-023-34250-4. PMID: 37120700; PMCID: PMC10148887.
- Updated U.S. Public Health Service guidelines for the management of occupational exposures to HIV and recommendations for postexposure prophylaxis.Personal Author(s) : Kuhar, David T.;Henderson, David K.;Struble, Kimberly A.;Heneine, Walid;Thomas, Vasavi;Cheever, Laura W.;Gomaa, Ahmed;Panlilio, Adelisa L.; Corporate Authors(s) : USPHS Working Group on Occupational Postexposure Prophylaxis.;National Center for Emerging and Zoonotic Infectious Diseases (U.S.). Division of Healthcare Quality Promotion.; Published Date: 9/25/2013 Update (May 23, 2018) URL: https://stacks.cdc.gov/view/cdc/20711.
- Taiwo O. Dental practice, human immunodeficiency virus transmission and occupational risks: views from a teaching hospital in Nigeria. Ann Med Health Sci Res. 2014 Jul; 4(Suppl 2): S94-8. doi: 10.4103/2141-9248.138020. PMID: 25184095; PMCID: PMC4145525.
- Recommendation for the application of post-exposure prophylaxis (PEP) against HIV infection. ” Official Gazette of the Republic of North Macedonia” No. 09-4576/2021; June p. 26- No. 148.
- URL: https://stanfordhealthcare.org/medical-conditions/sexual-and-reproductive-health/hiv-aids/diagnosis/western-blot-test.html.
Eyong EM, Ngwe NY, Nfuksai CN, Niba LL, Jane-Francis A. Prevalence of Occupational Exposure to HIV and Factors Associated with Compliance with Post-Exposure Prophylaxis Among Health Workers of the Biyem-Assi, Buea, and Limbe Health Districts of Cameroon Maternal and Child Health and AIDS. Int J MCH AIDS. 2022;11(1): e557. doi: 10.21106