UDK: 616.831-002-073.763.5:618.3
Mladenovikj Shumanov I.1, HadjiNikolova Alchinova N.2
1 City General Hospital “8th September”, Department of Radiology, Skopje
2 University Clinic of Radiology, Skopje
Abstract
Wernicke’s encephalopathy (WE) is a neurological condition caused by thiamine deficiency (vitamin B1) and it is the most commonly seen in chronic alcoholics. Other etiologies, connected to this pathology, are malnutrition, hemodialysis, gastrointestinal surgery, hyperemesis gravidarum (HG), etc. Clinical criteria of WE are altered mental status or memory impairment, oculomotor dysfunction and cerebellar dysfunction. Cerebral magnetic resonance is the diagnostic of choice. Wernicke’s encephalopathy in pregnancy is a result as a complication of HG.
We present a case of pregnant women in her 16th gestational week who was presented with consciousness impairment, nystagmus and ataxia, and suffered for a month before receiving her initial WE. As a diagnostic method, magnetic resonance of brain was performed with characteristic signs of WE.
Key Words
Case report, Hyperemesis gravidarum, Magnetic resonance, Radiology, Wernicke encephalopathy.
Introduction
Wernicke’s encephalopathy (WE) is a reversible rare neurological condition caused by hyperemesis gravidarum (HG) due to thiamine (vitamin B1) deficiency.
Chronic alcoholism (the mostcommon), Hyperemesis gravidarum, malnutrition, inflammatory bowel disease, etc., can lead to WE.
Clinical criteria of WE are characterized by mental status alteration, ophthalmoplegia, and ataxia triad. If there is one or two of the previous symptoms in correlation with clinical, laboratory and diagnostic findings, the diagnosis of WE can be confirmed. This case is to present the importance of MRI in early diagnosis of WE in pregnant women.
This is a case of women in her 2nd trimester of pregnancy with HG that developed the typical symptoms of WE and characteristic imaging findings on the brain imaging. On MRI, there are distinct pattern of alterations that include symmetrical alteration in the mamillary bodies, thalami, Tectal plate and periaqueductal area.
Case Presentation
A 38-years-old pregnant patient at 15 weeks and 6 days of gestational age, in her third pregnancy, presented with symptoms of weakness, spontaneous nystagmus, ataxia, mental confusion and amnesia.
One month before this visit, she was hospitalized for a week for extreme vomiting due to the Hyperemesis gravidarum.
Laboratory tests showed the following changes: thiamine level (50nmol/L), drop in hemoglobin levels (103mg/dl, reference: 120-180g/l), albumin (28g/l, reference: 35-52mg/dl), CRP (34 reference level <5) and increased liver enzymes AST (332U/L, reference 5-34U/L), ALT(523U/L, reference 9-55U/L) and LDH (363U/L, reference 125-220U/L).The other performed exams, did not show significant deviations. The ultrasound exam showed a live fetus.
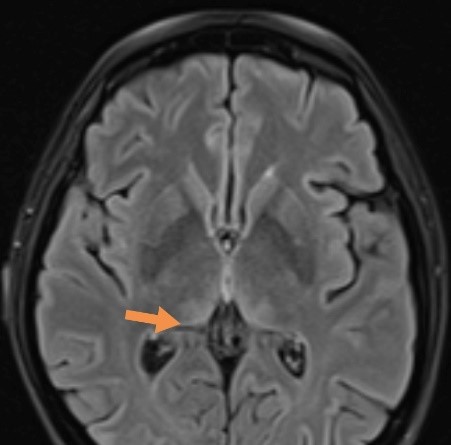
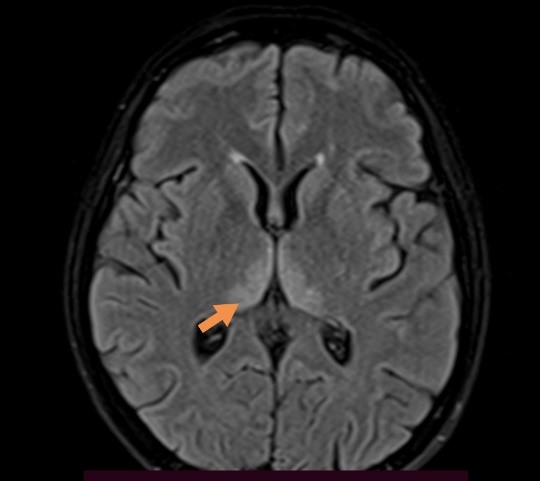
MRI of brain was obtained using postcontrast sequences with sagittal and axial T1, axial T2 and FLAIR and diffusion weighted imaging (DWI). On T2/FLAIR sequences there were hyperintensities in the medial part of both thalami and periaqueductal areas (Figure 1), which also showed DWI restriction – highly suggestive for of Wernicke´s encephalopathy (Figure 2).
 |
 |
| Figure 1. Presentation of hyperintensities in thalami and periaqueductal areas on MRI brain in T2/FLAIR sequence. | |
As a result of the clinical symptoms, laboratory analyses and the findings from the magnetic resonance, the diagnosis was in favor of WE, and intravenous administration of thiamine was initiated.
For the safety of the patient induced abortion was suggested and with consent of the mother, the abortion was performed.
During the time of hospitalization, an improvement in the patient`s condition was observed.
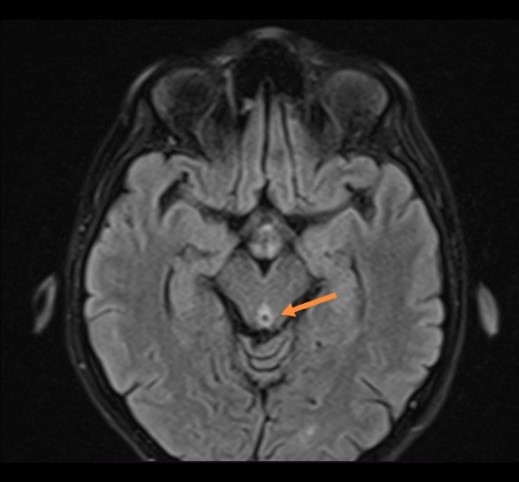
Control MRI of the brain was performed. This follow-up showed a resolution of previously bilateral hyper intense signals regions on T2/FLAIR sequence, with progressive reduction of hypersignal changes of bilateral thalamic regions of restricted diffusion (Figure 3).
| Figure 3. Presentation of reduction of hypersignal changes of bilateral thalamic regions on T2 FLAIR on MRI. |
Discussion
Hyperemesis gravidarum is a condition that occurs very frequently in early pregnancies and can lead to weight loss, malnutrition, dehydration, but in very rare cases can cause rare neurological complications as WE.
The patient in this case, presented with the triad of symptoms typical for WE: ataxia, spontaneous nystagmus, mental confusion, and previous history of hyperemesis gravidarum.
The laboratory results showed low levels of vitamin B1 and obtained MRI showed characteristic findings for WE.
The diagnosis of WE is based by clinical presentation, but the definitive diagnosis can be accomplished with MRI which shows bilateral symmetrical low T1, high T2 and FLAIR signal intensity with restricted diffusion of the medial thalami, periaqueductal area, mamillary bodies, etc.
The treatment should include a high dose of thiamine replacement.
Conclusion
WE as a complication of HG is rare neurological condition.
Small possibility of WE at pregnant patients should be treated immediately with thiamine iv administration. Undiagnosed WE could cause neurological morbidity and mortality.
The complementary approach of clinical exam, laboratory results and typical MRI findings lead to early recognition and better outcomes for the patients.
References:
- Harper C, Fornes P, Duyckaerts C, Lecomte et al: An international perspective on the prevalence of the Wernicke-Korsakoff syndrome. Metab Brain Dis. 1995, 10:17-24. 10.1007/BF01991779.
- Galvin R, Bråthen G, Ivashynka A, Hillbom M et al: EFNS guidelines for diagnosis, therapy and prevention of Wernicke encephalopathy. Eur J Neurol. 2010, 17:1408-1418. 10.1111/j.1468-1331.2010.03153.x.
- London V, Grube S, Sherer DM et al: Hyperemesis gravidarum: a review of recent literature. Pharmacology. 2017, 100:161-171. 10.1159/000477853.
- Lee NM, Saha S: Nausea and vomiting of pregnancy. GastroenterolClin North Am. 2011, 40:309-334. 10.1016/j.gtc.2011.03.009.
- Baba Y, Morisawa H, Saito K, at al : Intraperitoneal hemorrhage in a pregnant woman with hyperemesis gravidarum: vitamin K deficiency as a possible cause. Case Rep Obstet Gynecol. 2016, 2016:5384943. 10.1155/2016/5384943.
- Frank LL: Thiamin in clinical practice. JPEN J Parenter Enteral Nutr. 2015, 39:503-520. 10.1177/0148607114565245.
- Ashraf VV, Prijesh J, Praveenkumar R at al: Wernicke’s encephalopathy due to hyperemesis gravidarum: clinical and magnetic resonance imaging characteristics. J Postgrad Med. 2016, 62:260-263. 10.4103/0022-3859.191005.
- Berg JM, Tymoczko JL, Stryer L: Biochemistry: 5th Edition. W H Freeman, New York; 2002.
- Hazell AS, Butterworth RF: Update of cell damage mechanisms in thiamine deficiency: focus on oxidative stress, excitotoxicity and inflammation. Alcohol Alcohol. 2009, 44:141-7. 10.1093/alcalc/agn120.
- Suzuki S, Ichijo M, Fujii H at al: Acute Wernicke’s encephalopathy: comparison of magnetic resonance images and autopsy findings. Intern Med. 1996, 35:831-834. 10.2169/internalmedicine.35.831.