UDK: 618.14-007.21:618.5-089.888.61
Pregnancy in a Patient with a Congenital Unicorn Uterus and Conization Due to Cervical Cancer
Bushinoska Ivanova G.1, Bushinoska J.2, Ivanov J.2
1 Clinical Center “Mother Theresa”, University Clinic of Gynecology and Obstetrics, Skopje, Republic of North Macedonia
2 Acibadem Sistina Hospital, Skopje, Republic of North Macedonia
Abstract
Introduction: A unicornuate uterus can cause gynecological and obstetrical complications, such as hematometra, infertility, miscarriage and premature births. However, in some cases, despite the small capacity of unicornuate uterus, a successful pregnancy with the birth of a healthy and viable fetus is still possible, as in this case.
Case Report: We present a case of a 39-years-old patient, who delivered a fetus prematurely at 32 weeks of pregnancy, conceived by IVF. What is important about this case is that the patient had a congenital unicornuate uterus with a small capacity, and in which 18 months before conception, a conization was performed, due to a diagnosed carcinoma of the cervix. After conization and two negative Pap smears, after 8 months, the patient was suggested to start trying to get pregnant. Since there was no success with spontaneous pregnancy in the next 10 months, it was decided that the patient would become pregnant with an IVF procedure. The patient became pregnant during the first IVF attempt and after the first embryo transfer, the pregnancy began to develop successfully. At the beginning of pregnancy, the length of the cervix was 25mm. and the first shortening on the cervix was observed at 21st week of pregnancy, when the measured length was 20mm. Strict rest, progestogens and tocolytic therapy were indicated, with which the first contractions were delayed and appeared for the first time at 26th week of gestation. Two maturations of the fetal lung of the fetus with corticosteroids were carried out at 28 and 31 weeks of pregnancy, and due to increased contractions, the process of delivery began at 32nd week of pregnancy, when it was decided to end the birth by Caesarean section. The patient gave birth by caesarean section to a live male fetus weighing 1,345 grams and 40cm length and with APGAR score 6/7/7 at 32.2 gestational weeks. The caesarean section went without complications and the patient left the hospital three days after the operation. The newborn had a proper adaptation after delivery and was placed in the NICU, where he spent 29 days, without major complications, with spontaneous respirations only on the support of diffused oxygen in the first ten days.
Conclusion: Despite the fact that it is difficult to achieve a successful pregnancy with the birth of a live and healthy fetus in patients with congenital unicornuate uterus, and in this case complicated by shortening of the cervix before pregnancy due to conization, however, with good pregnancy management, delivery of a healthy fetus is possible in such cases as well. Even though the pregnancy in such cases cannot last until the due date, with timely prescription of corticosteroids and termination of the pregnancy to the maximum gestational week, a healthy and vital fetus can still be obtained.
Key Words: preterm delivery, unicorn uterus, conization, microinvasive carcinoma, caesarean section.
Introduction
Unicorn uteri account for 2-13% of all genital Müller duct anomalies occurring in women. Anomalies of the Müllerian ducts, such as a unicornuate, bicornuate, or septate uterus, occur in 5-10% of women of reproductive age who have had a miscarriage [1]. Uterine anomalies lead to spontaneous abortions, preterm births, fetal malpresentation, rupture of the amniotic fluid, placental abruption, increased number of caesarean sections and intrauterine fetal growth retardation [2, 3]. Only 29% of women with a unicornuate uterus give birth, and 44% end up giving birth prematurely [4, 5]. 24% of these pregnancies end with spontaneous abortion in the first trimester, and about 20% in the second trimester with the birth of immature fetuses [4-6,7]. In these pregnancies with a unicornuate uterus, there is a risk that a rupture of the horn may occur in over 50% of the patients, mostly at the end of the second trimester [8].
The use of progesterone in these pregnancies has been shown to be an important factor in maintaining these pregnancies, despite the fact that its effectiveness decreases with increasing of the gestational age [5].
Case Report
This is a case of pregnancy in a patient after conization and with a congenital unicornuate uterus with a small capacity, who carried the pregnancy and gave birth prematurely at 32 weeks of pregnancy.
A 37-year-old patient, without previous conception and childbirth, came for a consultation about getting pregnant, after two years of marriage. At the first consultation, a routine gynecological examination was performed, during which a Pap smear was taken, and an ultrasound of the genitals was performed, which detected a uterus with a smaller capacity and two ovaries of normal size and morphology.
The result of the Pap smear after one week showed a suspicion of squamous cell carcinoma, after which a colposcopy of the cervix was performed with a positive finding for a cancerous process on the posterior lip of the cervix, after which a biopsy of the cervix was indicated.
After a certain preparation of the patient, in the middle of the menstrual cycle and after the end of the patient’s menstruation, a biopsy of the cervix and endocervical curettage was performed and the obtained material was sent for histopathological analysis. The biopsy result showed squamous cell microinvasive carcinoma (T1A1). The obtained result of the biopsy indicated to make a diagnostic conization, as the next step.
The patient was prepared and the following month, conization with an ultrasound knife was performed, after which the histopathological diagnosis was confirmed for microinvasive squamous carcinoma of the cervix on the posterior lip, with the greatest depth of invasion up to 1mm, (PT1A1), and lines of the operative incision endo and exocervical passed through healthy tissue.
The patient’s condition was monitored postoperatively and after two Pap smears with good results and a colposcopy with good results, the patient was advised to try to get pregnant.
Next, an HSG (Figure 1) was performed, and it was confirmed that it was a congenital unicornuate uterus with only the right horn developed, with a normal right tube and agenesis of the left tube and with one cervix.
There were also two unsuccessful inseminations after one year of conization of the patient.
After 18 months without successful conception, it was decided to implement a stimulation protocol for the patient and IVF. After the stimulation protocol was performed, the patient’s follicles were punctured, 3 oocytes were obtained, two of which were fertilized, and it was decided to return only one embryo with embryo transfer to the right horn of the patient’s uterus.
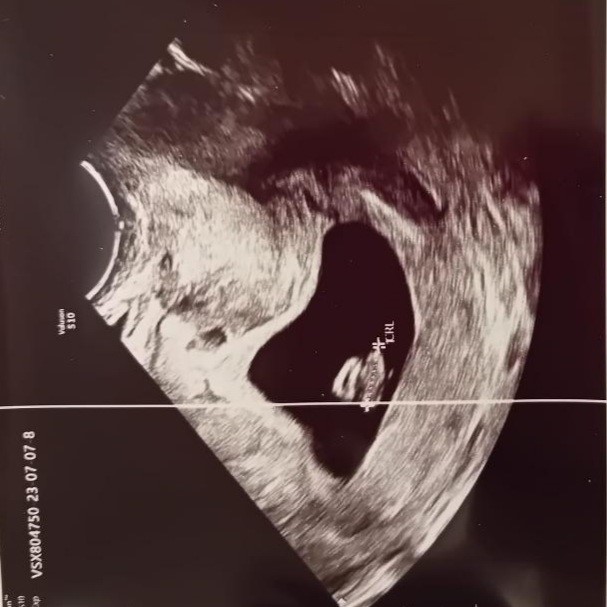
After two weeks of the embryo transfer, we received a positive pregnancy test and after 4 weeks of the embryo transfer, a vaginal ultrasound detected a fetus in the uterus, with a positive heartbeat (Figure 2).
Figure 1. HSG- hysterosalpingography. Figure2. Pregnancy detection with US.
The pregnancy was managed actively, with frequent controls and monitoring of the growth and progress of the fetus, as well as with measurements of the cervix, which was shortened and 25mm long from the beginning of the pregnancy, due to a previous conization of the patient.
The pregnancy was monitored by protocol with all: ultrasound, biochemical, infectious and genetic screenings. During the entire pregnancy, progesterone was administered orally and vaginally to the patient, as well as magnesium and with a recommendation for strict rest.
Ultrasound examinations monitoring of fetal growth and development and cervical length were performed every 2-3 weeks. Detailed ultrasound screenings of the fetus were performed in the first (Figure 3) and second trimesters (Figure 4) of pregnancy, infectious screenings by taking microbiological smears and serological analyzes at the end of the first trimester in the 12th week of gestation, biochemical investigations and genetic screening due to the mother’s age – 39 years were performed, and were with normal finding.
Figure 3. US screening in 1st trimester. Figure 4. US screening in 2nd trimester.
The patient was also monitored for laboratory analyses, glycemia and blood pressure measurement during pregnancy, which fortunately were normal all the time and were not a factor in complicating the pregnancy.
In the 15th week of pregnancy, the cervix was 25mm long, it had not been further shortened since the beginning of pregnancy, and therefore it was decided not to place a cerclage, but to intensively monitor and treat infections during pregnancy, which can lead to shortening of the cervix and also to prevent its shortening of the cervix by local and systematic use of progestogens.
At 21st week of pregnancy, the first shortening of the cervix by 5mm was observed, and the cervix was 20mm long. The patient was advised to have further therapy with progestogens, tocolytics and strict rest.
The first mild contractions of the uterus appeared in the 26th week of pregnancy, and the first ripening with corticosteroids, for pulmonary ripening due to the risk of premature birth, was carried out in the 28th week of pregnancy.
Measurements of the length of the cervix showed 15mm, and further strict rest, progestogen therapy and tocolytics were advised. The contractions continued and the second ripening was carried out at 31st week and due to the strong contractions and the opening of the cervix of 3cm, it was decided to end the delivery by Caesarean section at 32.2 weeks of pregnancy.
The patient gave birth by caesarean section at Gynecology and Obstetrics Clinic in Skopje, to a live male fetus with weight 1,345 grams and 40cm length and with APGAR score 6/7/7. The caesarean section went without complications and the patient left the hospital three days after the operation. The newborn had a proper adaptation after delivery and was placed in the NICU, where he spent 29 days, without major complications, with spontaneous respirations only on the support of diffused oxygen inthe first ten days.
The newborn developed a neonatal infection that was treated with an antibiotic and jaundice that was treated with hydration and ultraviolet lamp tanning. The newborn at discharge from the hospital, after spending 29 days in the OINT after delivery, had a developed sucking reflex and weighed 1,850g, with advised regular neonatological controls.
Discussion
This is a successful pregnancy story, in a mother with congenitally small uterine capacity – a unicorn uterus and a shortened cervix due to a conization performed before pregnancy. With good preparation of the patient, despite the small capacity of the uterus and short cervix, as well as good management during pregnancy, with appropriate examinations, therapy and rest during pregnancy, all led to a successful end of pregnancy, with premature delivery of a healthy newborn [4, 5].
With a small capacity of the uterus and a shortened cervix and with the entire regime that was imposed on the patient during the pregnancy by the doctors who managed the pregnancy, with timely maturation with corticosteroids for pulmonary maturity, the maximum delay of the pregnancy was reached until 32nd gestational week and finished with premature delivery with viable fetus.
In these patients, spontaneous abortions and premature termination of pregnancies even before the end of the second trimester, with the birth of immature fetuses, which are not capable of life, are common [2, 3].
Ultrasound and imaging techniques in such cases are essential as diagnostic methods in pregnancy planning and management, as well as for monitoring the growth and development of the fetus in the uterus, as well as for measuring the cervix.
Conclusion
Despite the fact that it is difficult to achieve a successful pregnancy with the birth of a live and healthy fetus, in patients with congenital unicorn uterus, and in this case complicated by shortening of the cervix before pregnancy due to conization, however, with good pregnancy management, delivery of a healthy fetus is possible in such cases as well. Even though the pregnancy in such cases cannot last until the due date, with timely prescription of corticosteroids and termination of the pregnancy to the maximum gestational week, a healthy and vital fetus can still be obtained.
References:
- Chan YY, Jayaprakasan K, Tan A, Thornton JG, Coomarasamy A, Raine-Fenning NJ. Reproductive outcomes in women with congenital uterine anomalies: a systematic review. Ultrasound Obstet Gynecol. 2011;38:371–382. doi: 10.1002/uog.10056. [PubMed] [CrossRef] [Google Scholar].
- Hua M, Odibo AO, Longman RE, Macones GA, Roehl KA, Cahill AG. Congenital uterine anomalies and adverse pregnancy outcomes. Am J Obstet Gynecol. 2011;205(6):558. e1–e5. [PubMed] [Google Scholar].
- American Congress of Obstetrics and Gynecology Committee on Practice Bulletins- Obstetrics. ACOG practice bulletin: intrauterine growth restriction. Obstet Gynecol. 2000;95(Suppl):1–12. [Google Scholar].
- Akar ME, Bayar D, Yildiz S, Ozel M, Yilmaz Z. Reproductive outcome of women with unicornuate uterus. Aust N Z Obstet Gynaecol. 2005;45(2):148–150. doi: 10.1111/j.1479-828X.2005.00346.x. [PubMed] [CrossRef] [Google Scholar].
- Norwitz ER, Phaneuf LE, Caughey A. Progesterone supplementation and the prevention of preterm birth. Rev Obstet Gynecol. 2011;4(2):60–72. [PMC free article] [PubMed] [Google Scholar].
- Reichman D, Laufer MR, Robinson BK. Pregnancy outcomes in unicornuate uteri: a review. Fertil Steril. 2009;91(5):1886–1894. doi: 10.1016/j.fertnstert.2008.02.163. [PubMed] [CrossRef] [Google Scholar].
- Grimbizis GF, Campo R, Gordts S, Brucker S, Gergolet M, Tanos V, Li T-C, De Angelis C, Di Spiezio Sardo A. On behalf of the Scientific Committee of the Congenital Uterine Malformations (CONUTA) common ESHRE/ESGE working group. Clinical approach for the classification of congenital uterine malformations. Gynecol Surg. 2012;9:119–129. doi: 10.1007/s10397-011-0724-2. [PMC free article] [PubMed] [CrossRef] [Google Scholar].
- Rackow BW, Arici A. Reproductive performance of women with müllerian anomalies. Curr Opin Obstet Gynecol. 2007;19(3):229–237. doi: 10.1097/GCO.0b013e32814b0649. [PubMed] [CrossRef] [Google Scholar].