UDK: 616-056.7:616.22-072.1]-053.31
Ognjanova Simjanovska V2, Donev Lj1,2, Golubic Nichevska S2, Angjusev D1,2, Leshi A1,2
1Faculty of Medicine, “Ss. Cyril and Methodius” University, Skopje, Macedonia,
2KARIL, TOARILUC, Skopje, Macedonia.
Abstract
Pierre Robin Syndrome (PRS) is characterized by a sequence of events including mandibular hypotrophy (micrognathia), abnormal posterior placement of tongue (glossoptosis) and airway obstruction. Pyloric Stenosis, on the other hand, is the most common infant surgical condition which presents with episodes of projectile vomiting leading to dehydration and weight loss. Airway management in these patients is a true challenge for every anesthesiologist. The patient was 7 weeks old infant, weighted 3.1kg, admitted in Intensive Care Department for surgical repair of pyloric stenosis, previously diagnosed with Pierre Robin Syndrome at birth. Preoperative preparation, intravenous rehydration and electrolyte substitution was obtained. Video-laryngoscope was used for management of difficult airway. We had many attempts in visualization of the vocal cords, eventually we performed awake intubation with stylet uncuffed endotracheal tube size 3. Pyloromyotomy was performed. The maintenance of anesthesia was with Sevoflurane and bolus doses of Fentanyl as adjunct. The perioperative vital signs were within normal ranges. Awake extubating was performed. The facial malformation that appears in patients with Pierre Robin Syndrome makes visualization of the glottis extremely difficult to impossible. In cases where tracheal intubation is needed, awake fiberoptic intubation is recommended, but it can have many limitations. These two conjoined conditions present the quandary of safely managing an expected difficult airway in an uncooperative patient. With this case we can conclude that for children with Pierre Robin Syndrome, video-laryngoscopy should be considered as the first attempt intubation device both in the operating room and for emergent situations.
Key Words: Difficult airway, Pierre Robin, pediatric, video-laryngoscopy.
Introduction
Pierre Robin Syndrome is estimated to affect 1:8,500 live births. It is characterized by micrognathia, glossoptosis and U-shaped cleft palate. Pierre Robin sequence can be found in isolation or in association with other congenital anomalies (1).. Pyloric stenosis, on the other hand, is one of the most common infant surgical conditions with an incidence of approximately 1/400 live births. It is presented with persistent and frequently projectile episodes of vomiting, which in severe cases can lead to dehydration, hypovolemia and weight loss. This condition regarding difficult airway, especially conjoined with pyloric stenosis, is a real challenge for anesthesiologists (2).
Case Report
We present a case of a 7-weeks-old infant, weight 3.1kg, admitted in the intensive Care Department for surgical repair of pyloric stenosis (pyloromyotomy). The patient was diagnosed with Pierre Robin Syndrome and Pyloric Stenosis shortly after birth. Previously the patient was hospitalized two times with episodes of vomiting and diarrhea in the last three weeks and weight loss of approximately 20%. Preoperatively, echocardiography was obtained (normal findings, closed fetal communications), fiber nasal laryngoscopy was with the following findings: present cleft palate defect, omega shaped epiglottis and visible larynx. On admission the patient was hemodynamically and respiratory relatively stable with following parameters: Blood Pressure (BP) 100/74; Heart Rate (HR)152, SpO2=98%. Arterial Blood Gas Analysis showed Hypokalemia, Hyponatremia with metabolic alkalosis. The skin was pale with decreased turgor and elasticity. Nasogastric tube was placed, intravenous rehydration with electrolyte substitution were ordinated.
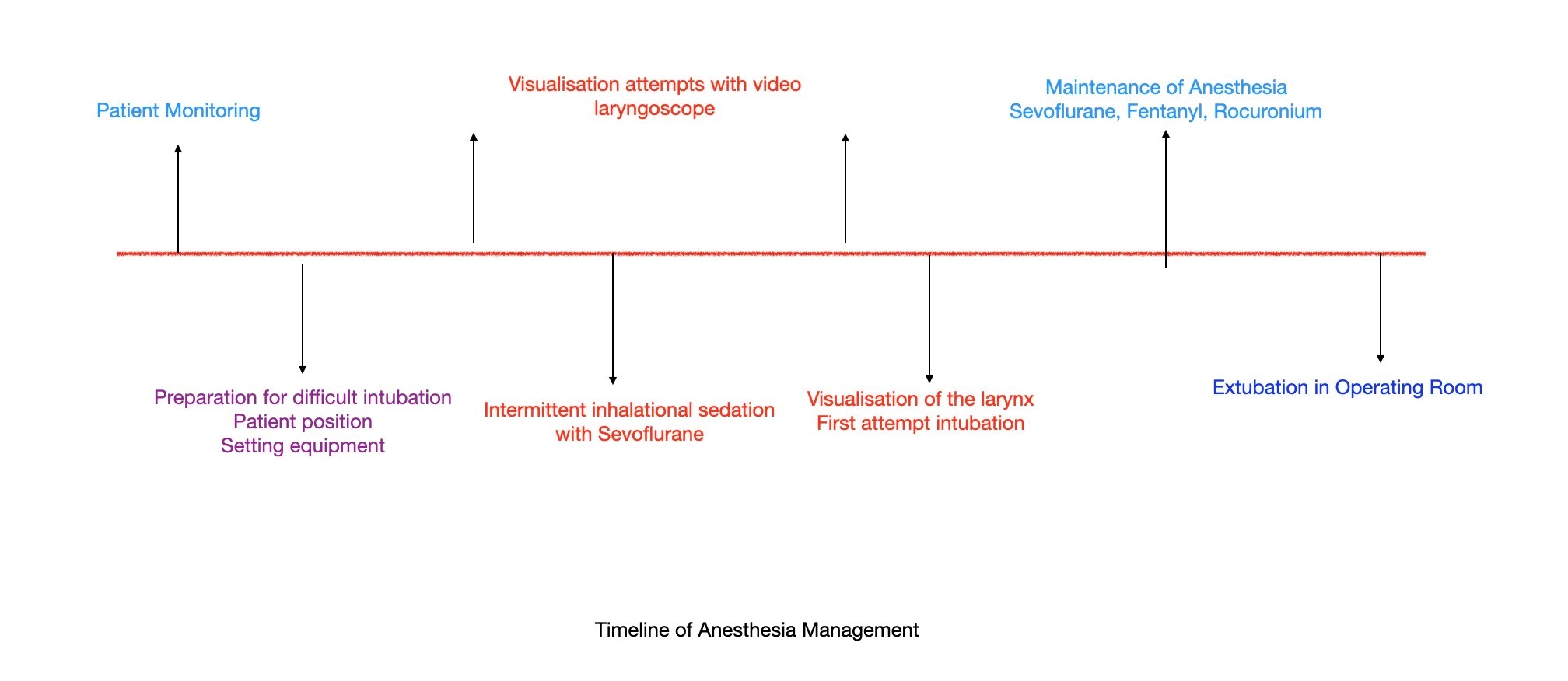
The patient was admitted at the Operating Room and preoperative preparation was obtained. The patient was placed in supine position and standard monitoring was placed (EKG, Blood Pressure, Pulse oximeter and temperature monitor). We used video-laryngoscope for difficult airway management. We inserted the video-laryngoscope blade, first we had difficulties in obtaining visualization of the larynx. After many attempts we performed awake intubation with 90° angled stylet endotracheal uncuffed tube, size 3. Sevoflurane was used for maintenance of anesthesia with 2μg/kg/fentanyl as adjunct. Acetaminophen 7.5mg/kg was given intraoperatively to supplement opioid analgesia. Perioperative fluid therapy with normal saline of 15ml/kg/hour was maintained. Urine output was measured (maintained > 1ml/kg/h) and air warmer was used to preserve normothermia. Perioperative vital parameters were within normal range. After fully emerged from general anesthesia, awake extubating was performed.
Discussion
Pierre Robin Syndrome (PRS) is characterized by a sequence of events including mandibular hypotrophy (micrognathia), abnormal posterior placement of tongue (glossoptosis) and airway obstruction (3). The incidence of Pierre Robin sequence varies equally in boy and girl infants4. The underlying abnormality is thought to be hypoplasia of the mandible prior to 9 weeks gestation, that leads to displacement of the tongue posteriorly and superiorly between the palatal shelves preventing their fusion. Individuals with this defect are known to have difficult airway, and often experience airway obstruction, especially in the supine position. The airway is believed to become easier to manage with increasing age.
Pyloric stenosis, on the other hand, is one of the most common infant surgical conditions with an incidence of approximately 1/400 live births. It is presented with persistent and frequently projectile episodes of vomiting, which in severe cases can lead to dehydration, hypovolemia and weight loss. This condition is associated with hypochloremic hypokalemic metabolic alkalosis and compensatory respiratory acidosis. Clinical presentation of pyloric stenosis is usually seen in infants between the second and eighth week after birth. Infants with pyloric stenosis are considered to be at risk for aspiration secondary to their gastric outlet obstruction in addition to the other recognized risks associated with anesthesia for this age group (2).
Pierre Robin Syndrome and Pyloric Stenosis as two conjoined conditions present the quandary of safely managing an expected difficult airway in an uncooperative patient.
The facial malformation that appears in patients with Pierre Robin Syndrome makes visualization of the glottis extremely difficult to impossible. In cases where tracheal intubation is needed, awake fiberoptic intubation is recommended, especially fiberoptic intubation through laryngeal mask (for children under 1 year old). However, there are several limitations like longer training and longer learning curve, expensive equipment and maintenance (5).
At our institution, commonly we use video-laryngoscope for managing difficult airway in pediatric patients. It this case we found it proper, with preparation of other equipment according to the difficult airway guidelines. Some studies showed that it is more difficult to insert an endotracheal tube (ETT) through video-laryngoscopy because the blade of a video laryngoscope has much greater curvature than one of a conventional direct laryngoscope (5). The challenges that we met were the following: time to proper visualization of the glottis, time to intubate and time to ventilate, conjoined with higher oxygen consumption and faster oxygen desaturation. The first challenge was the most difficult, the time for proper visualization was longer than 120 seconds followed with many attempts. Meanwhile, intermittent ventilation with Sevoflurane for light sedation was performed. As soon as proper visualization was made, we inserted 90° angled stylet ETT on the first attempt without any difficulties. Correct placement of the ETT was further confirmed by auscultation and end-tidal CO2 detection. Because of the many attempts, we faced a problem regarding soft tissue trauma with minor edematous changes which we managed with intravenous application of methylprednisolone 1mg/kg perioperatively. After fully emerged grom general anesthesia awake extubating was performed. The patient was stable in the postoperative period, with stable vital parameters, no significant changes or problems with breathing, normal SpO2 during whole period in the ICU department. With this case we can conclude that for children with Pierre Robin Syndrome, even though fiberoptic intubation is recommended as the first choice in difficult airway management, it regards many limitations, and video-laryngoscopy should be considered as the first attempt intubation device both at the operating room and for emergent situations (6).
Conclusion
Patients with Pierre Robin Syndrome with the variety of complexity and intensity of concomitant problems can have a destructive impact on the child. Even after transitioning home, breathing and feeding problems may cause substantial distress to both the involved infants and their families. There are many underlying syndromes, both cardiological and neurologically associated with PRS. In one study it is shown that the mortality rate is 10% in patients with PRS in presence of neurological anomalies (8).
The cleft palate repair in this patient was recommended for later surgical intervention when the patient turns 12 months. Some studies showed that patients with Pierre Robin Syndrome had worse speech outcomes after cleft palate repair (7). A multidisciplinary approach should be obtained in all infants born with this condition, including genetic testing and examination of neurological anomalies. On the other hand, when diagnosed early, pyloric stenosis has an excellent prognosis. In this case, the patient was discharged after 5 days in good condition, well hydrated with maintained feeding tolerance.
References
- Gangopadhyay N, Mendonca DA, Woo AS. Pierre robin sequence. Semin Plast Surg. 2012 May;26(2):76-82. doi: 10.1055/s-0032-1320065. PMID: 23633934; PMCID: PMC3424697.
- Sharma KK, Agrawal P, Toshniwal H. Acquired gastric outlet obstruction during infancy and childhood: a report of five unusual cases. J Pediatr Surg. 1997 Jun;32(6):928-30. doi: 10.1016/s0022-3468(97)90654-0. PMID: 9200104.
- Mackay DR. Controversies in the diagnosis and management of the Robin sequence. J Craniofac Surg. 2011 Mar;22(2):415-20. doi: 10.1097/SCS.0b013e3182074799. PMID: 21403570.
- Vatlach S, Maas C, Poets CF. Birth prevalence and initial treatment of Robin sequence in Germany: a prospective epidemiologic study. Orphanet J Rare Dis. 2014 Jan 17; 9:9. doi: 10.1186/1750-1172-9-9. PMID: 24433508; PMCID: PMC3899445.
- Korean Journal of Anesthesiology 2014;66(4):310-313.Case Report. doi: https://doi.org/10.4097/kjae.2014.66.4.310.
- Peterson JD, Puricelli MD, Alkhateeb A, Figueroa AD, Fletcher SL, Smith RJH, Kacmarynski DSF. Rigid Video Laryngoscopy for Intubation in Severe Pierre Robin Sequence: A Retrospective Review. Laryngoscope. 2021 Jul;131(7):1647-1651. doi: 10.1002/lary.29262. Epub 2020 Dec 10. PMID: 33300625.
- Stransky C, Basta M, Solot C, Cohen M, Low DW, Larossa D, Jackson O. Do patients with Pierre Robin sequence have worse outcomes after cleft palate surgery? Ann Plast Surg. 2013 Sep;71(3):292-6. doi: 10.1097/SAP.0b013e3182898712. PMID: 23676521.
- Logjes RJH, Haasnoot M, Lemmers PMA, Nicolaije MFA, van den Boogaard MH, Mink van der Molen AB, Breugem CC. Mortality in Robin sequence: identification of risk factors. Eur J Pediatr. 2018 May;177(5):781-789. doi: 10.1007/s00431-018-3111-4. Epub 2018 Feb 28. PMID: 29492661; PMCID: PMC5899115.